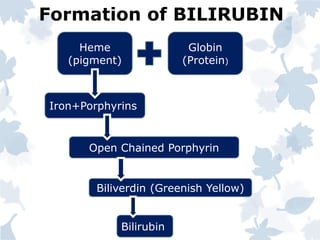
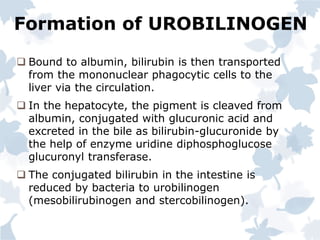
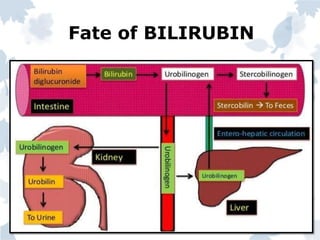
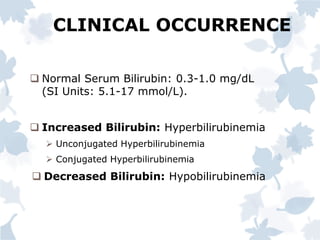
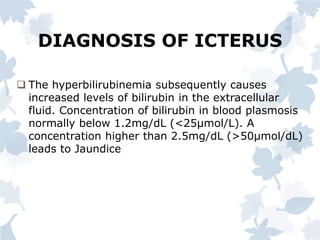
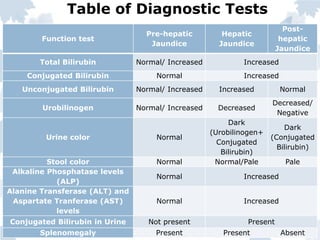
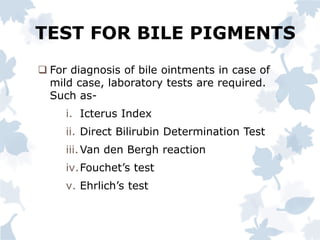
Bile pigments like bilirubin and biliverdin are produced from the breakdown of hemoglobin. Bilirubin is transported to the liver bound to albumin and conjugated with glucuronic acid before being excreted in bile. Elevated levels of bilirubin in blood causes jaundice. Jaundice can be prehepatic from excessive hemolysis, hepatic from liver toxicity, or posthepatic from biliary obstruction. Diagnosis involves liver function tests to differentiate the type based on conjugated and unconjugated bilirubin levels, urine and stool color, and other markers.