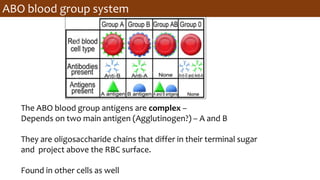
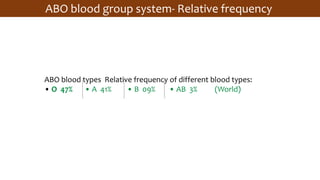
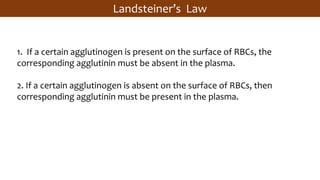
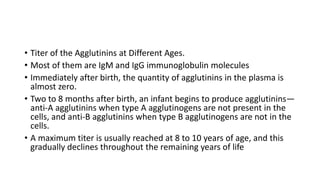
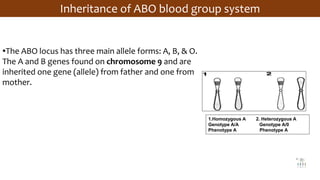
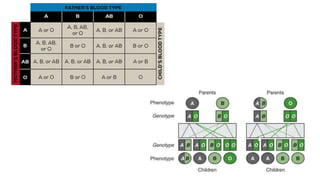
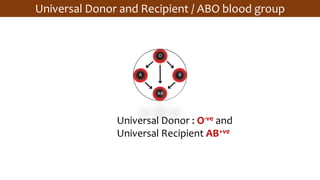
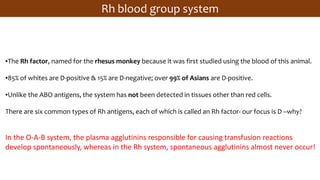
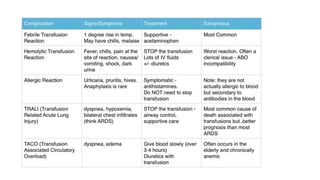
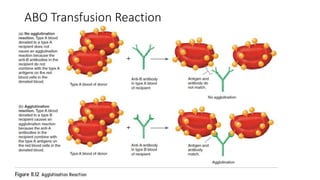
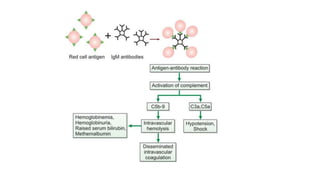
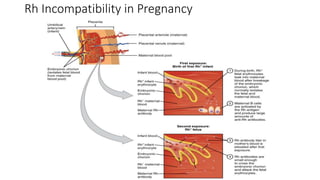
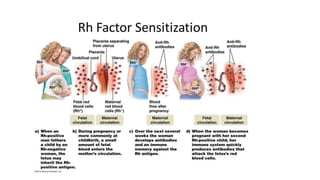
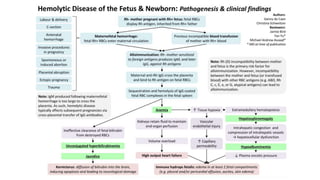
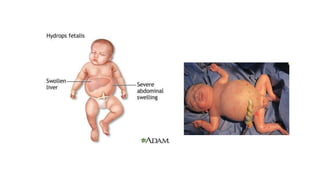
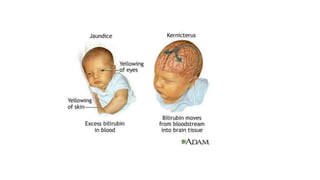
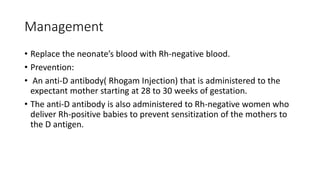
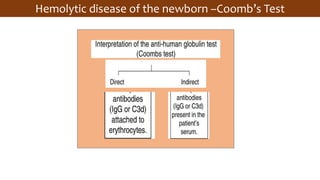
- The document describes the ABO and Rh blood group systems, including their patterns of inheritance and importance in blood transfusions and pregnancy. It discusses how blood type is determined by antigens on red blood cells and corresponding antibodies in plasma. ABO incompatibility can cause agglutination and hemolysis, while Rh incompatibility can cause hemolytic disease of the newborn. Proper blood typing and antibody screening can prevent transfusion reactions, and RhIg administration can prevent maternal sensitization and hemolytic disease in subsequent Rh-positive pregnancies.