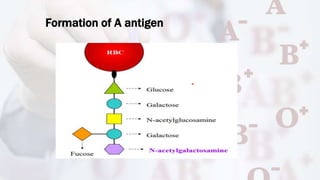
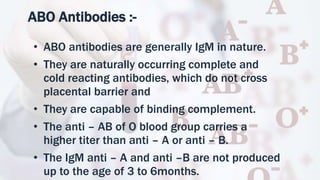
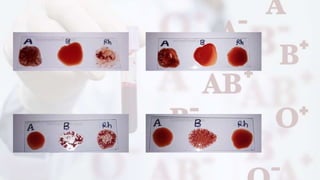
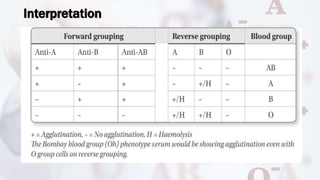
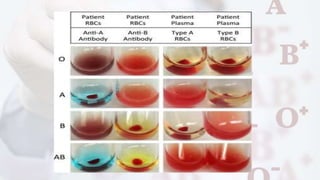
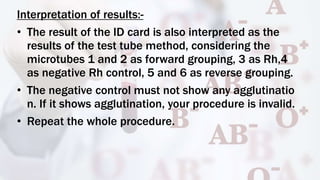
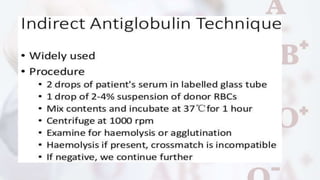
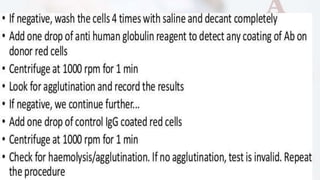
The document provides a comprehensive overview of blood grouping and cross-matching, focusing on various blood group systems, particularly the ABO and Rh systems, which are crucial for blood transfusions. It explains the genetics behind these blood groups, methods for testing blood types, and the clinical significance of different blood group subtypes, including the rare Bombay blood group. The document also details procedural techniques for conducting blood grouping tests and cross-matching to ensure compatibility before transfusions.