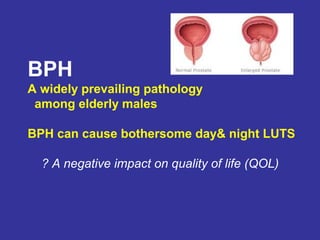
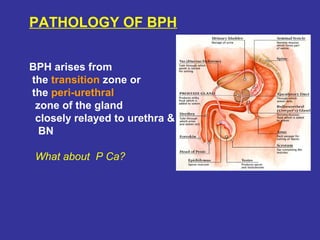
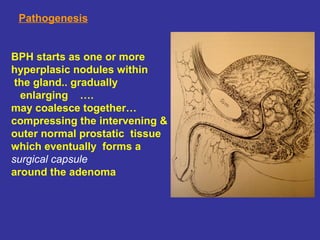
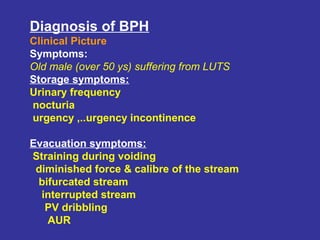
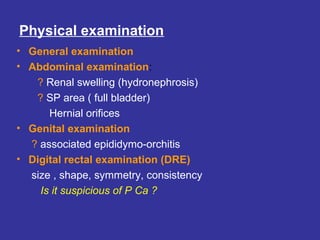
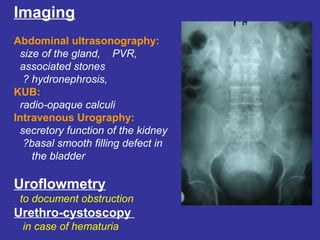
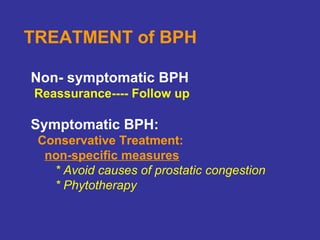
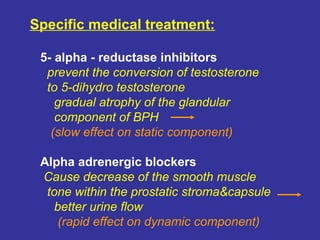
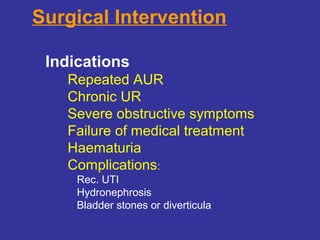
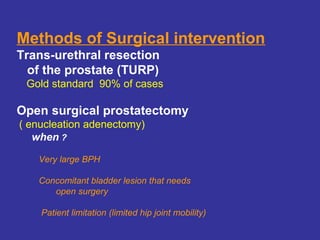
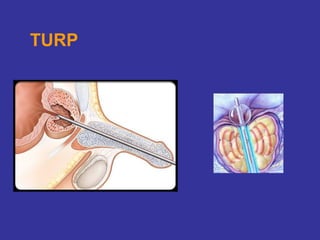
BPH is a common condition among elderly males that results from abnormal proliferation of the prostate's three histological elements. It causes bothersome lower urinary tract symptoms that negatively impact quality of life. Diagnosis involves evaluating an older man's symptoms and conducting a digital rectal exam and imaging tests. Most cases are treated initially with medications, while surgical intervention with TURP is recommended for severe, refractory, or complicated cases.