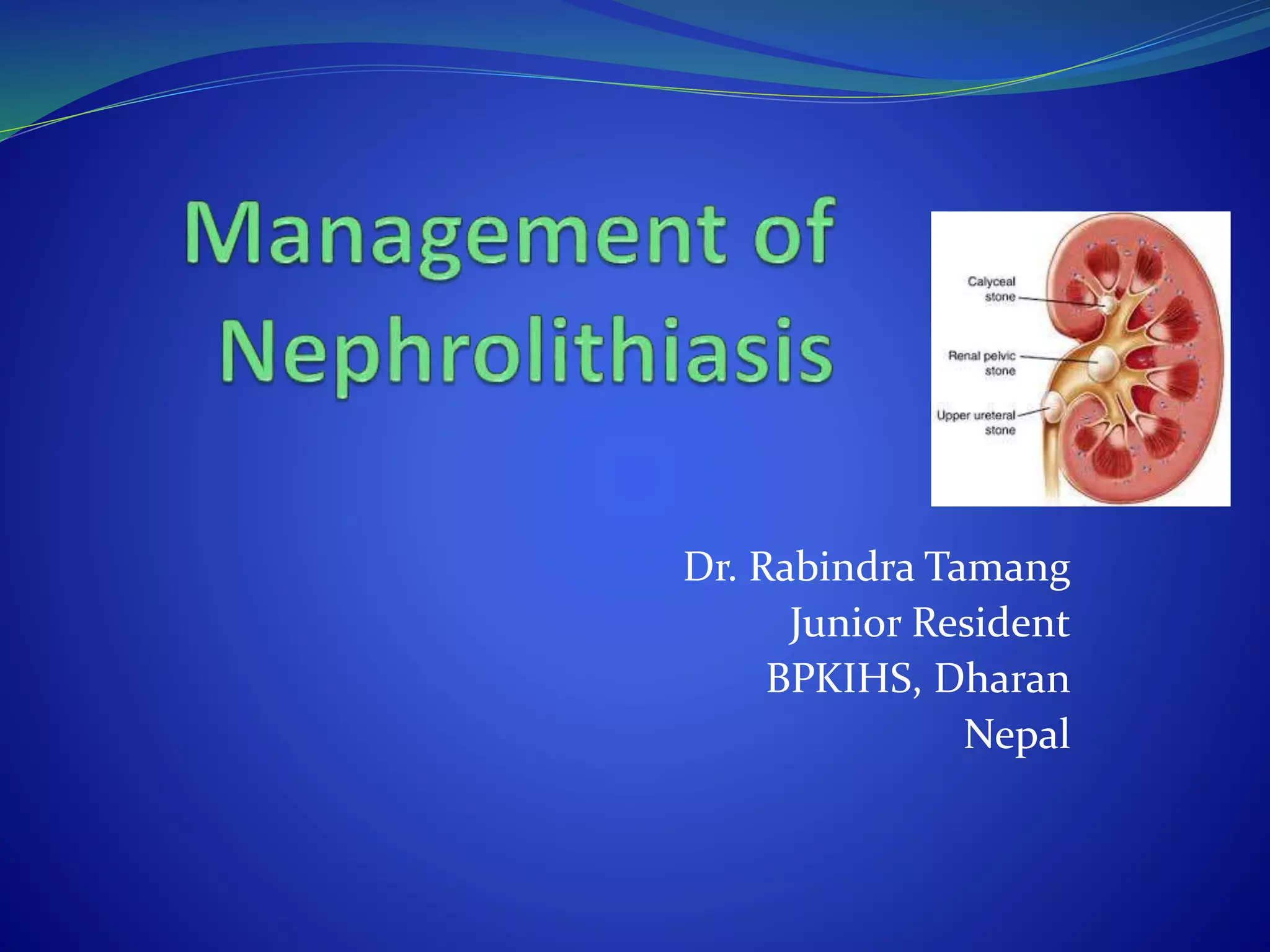
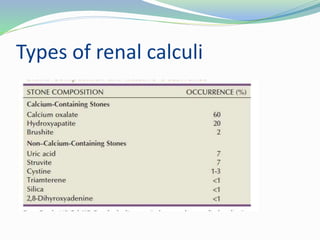
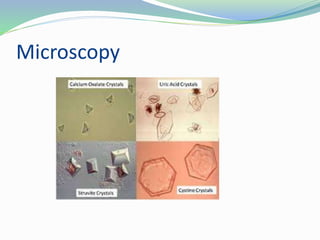
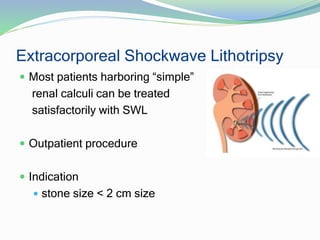
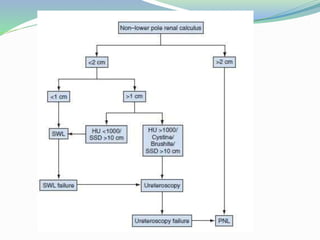
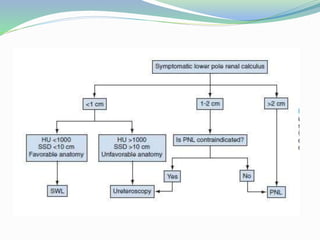
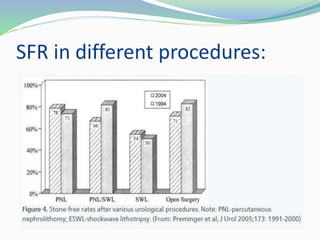
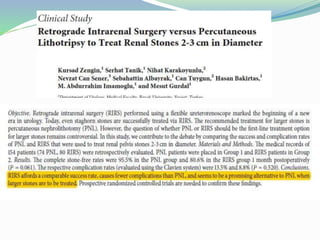
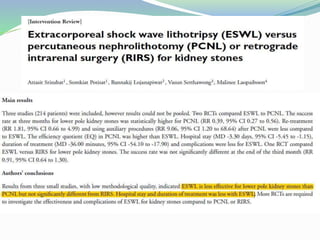
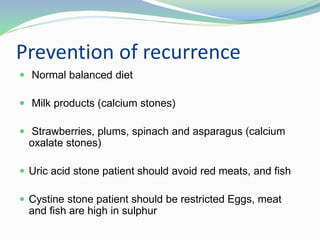
The document discusses nephrolithiasis, including its types, diagnostic evaluations, and management strategies. It covers both conservative and surgical treatments, emphasizing the importance of metabolic evaluations and tailored dietary recommendations to prevent recurrence. The conclusion highlights that while clinical symptoms often guide diagnosis, confirmatory tests and interventions are essential for larger stones.