The document provides an overview of liver function tests (LFTs), including their use, limitations, classification, and interpretation. Some key points:
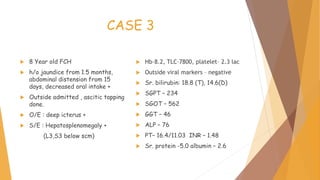
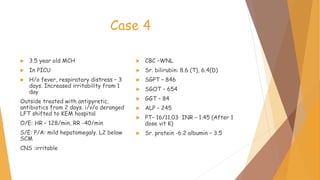
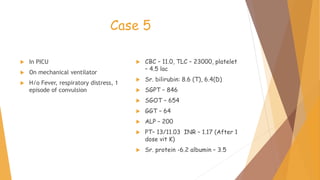
- LFTs evaluate liver biochemistry and injury but cannot detect overall liver function. Clinical history is most important.
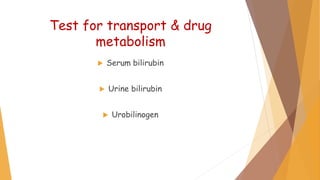
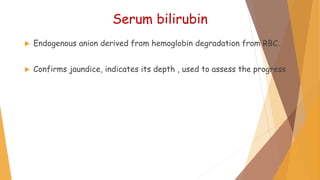
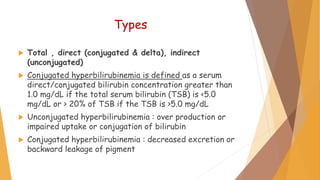
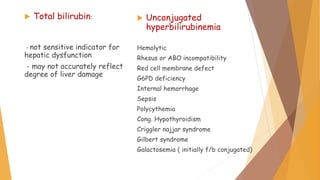
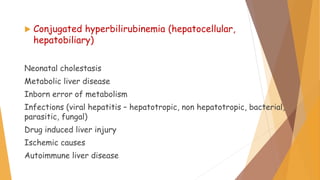
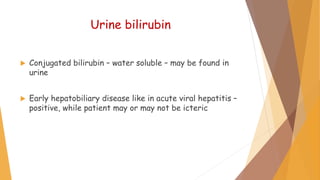
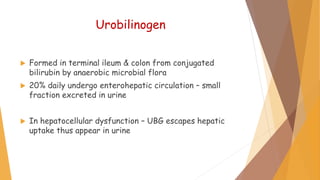
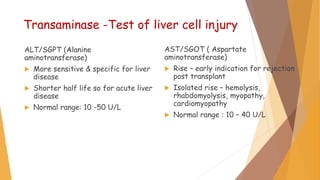
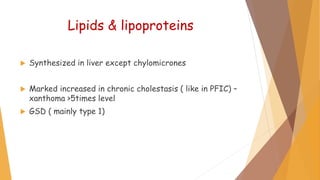
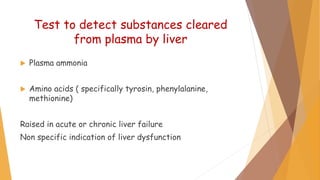
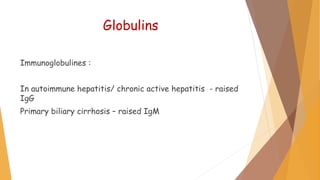
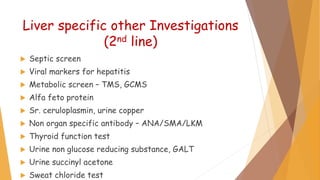
- Tests evaluate transport, injury, cholestasis, synthetic function, and substances cleared by the liver.
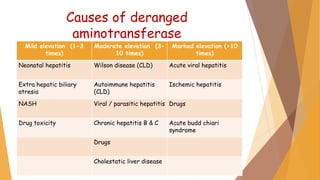
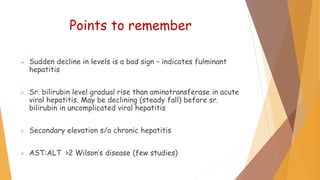
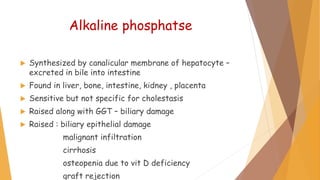
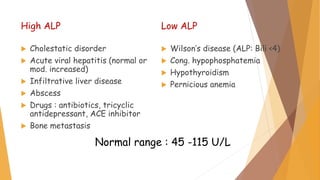
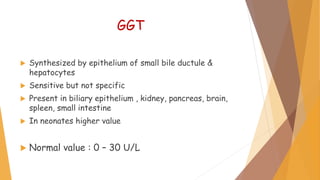
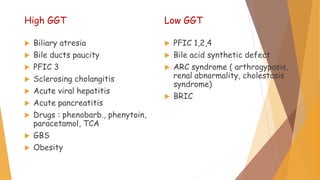
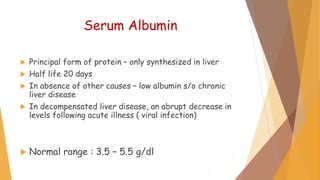
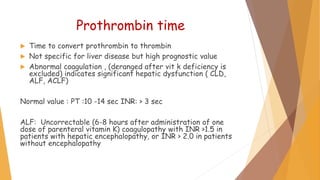
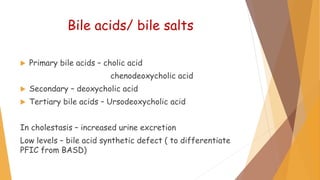
- Elevated enzymes like ALT/AST indicate liver cell injury while alkaline phosphatase and GGT indicate cholestasis. Albumin and PT assess synthetic function.
- LFTs can screen for disease, assess severity, and monitor treatment response but lack full sensitivity and specificity. Clinical context is critical for interpretation.