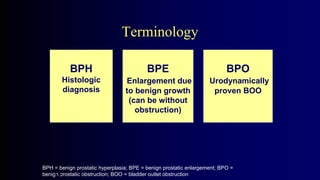
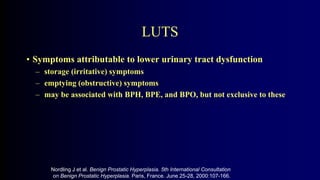
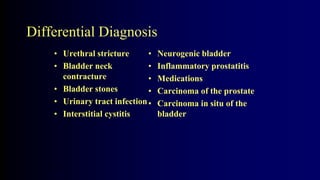
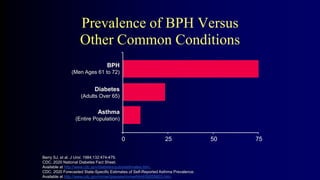
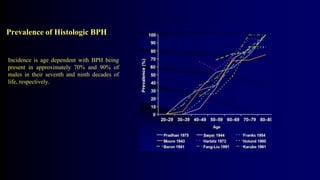
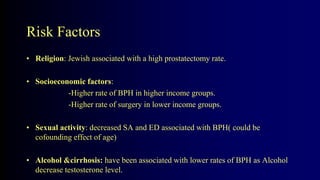
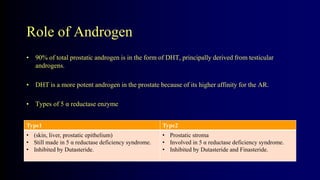
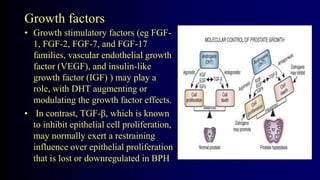
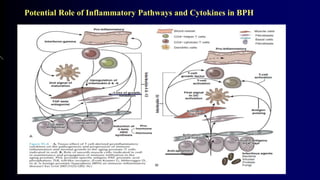
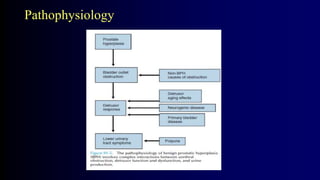
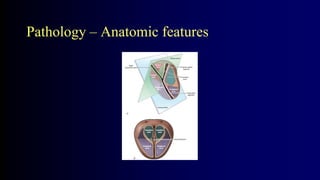
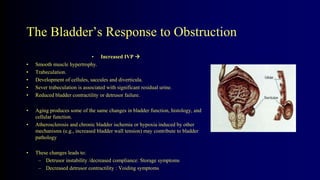
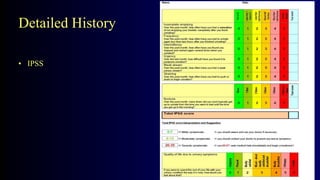
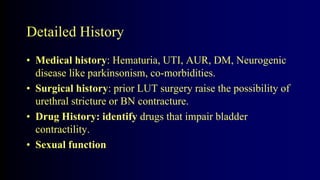
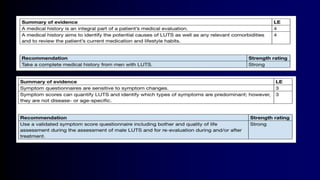
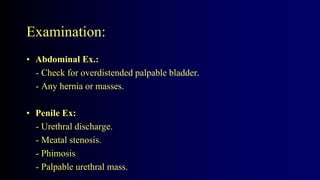
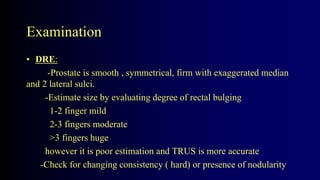
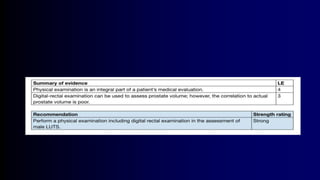
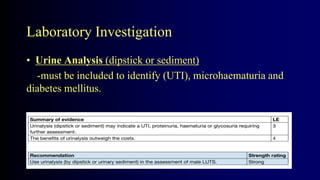
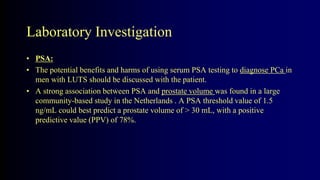
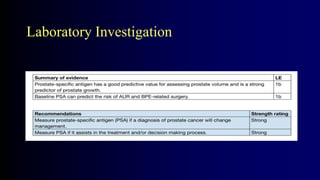
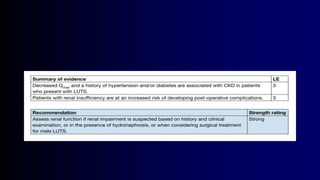
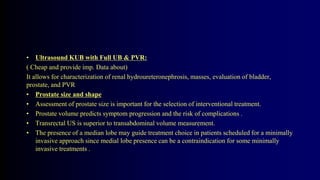
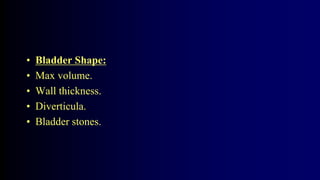
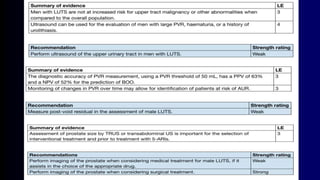
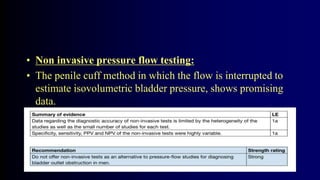
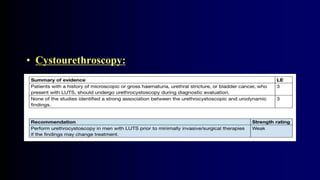
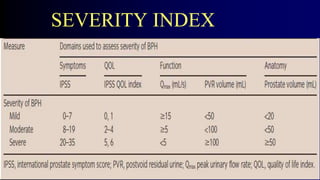
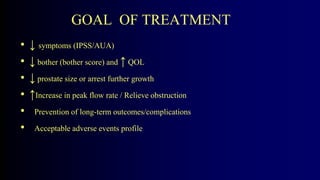
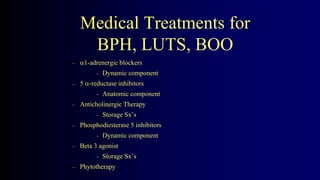
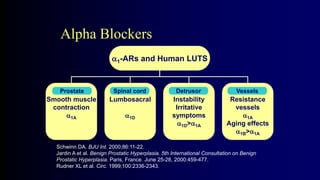
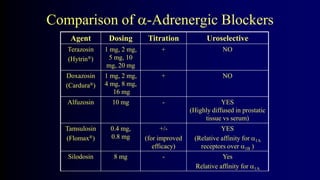
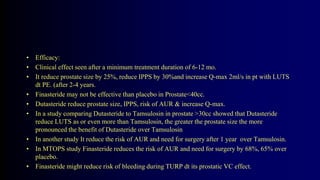
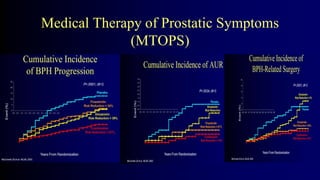
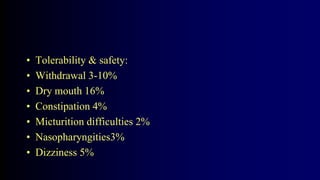
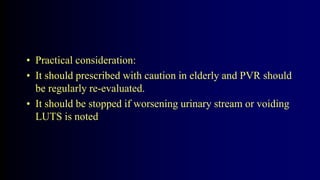
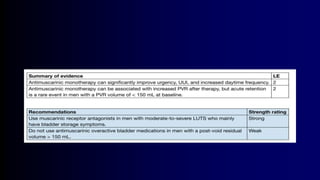
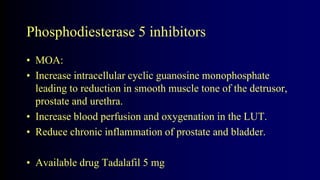
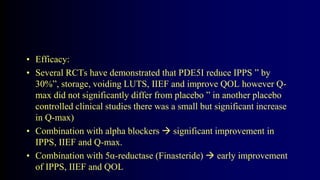
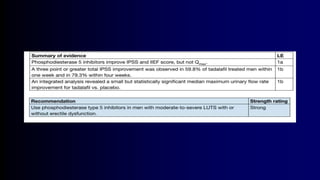
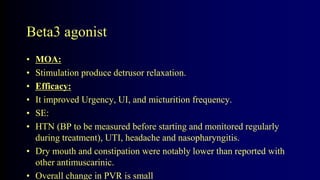
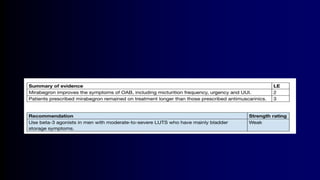
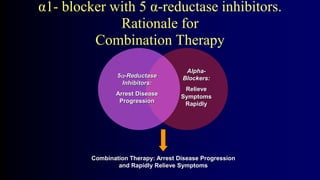
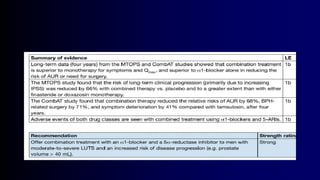
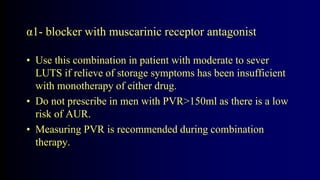
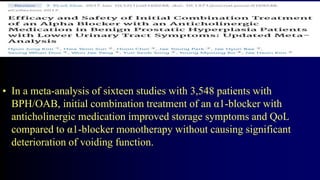
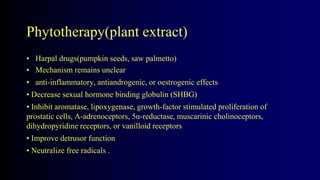
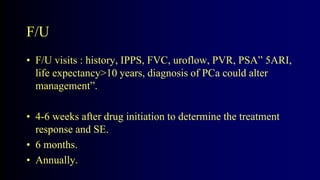
Benign Prostate Hyperplasia: Aetiology, Pathology , Diagnosis and Medical therapy is a document that discusses benign prostate hyperplasia (BPH). It covers the etiology, pathology, diagnosis, and medical therapy of BPH. The document discusses risk factors for BPH like age, genetics, and hormones. It describes the pathological features of BPH including epithelial and stromal cell hyperplasia. Diagnosis involves history, exam, lab tests like PSA and ultrasound. Medical therapy options presented are watchful waiting, alpha blockers, 5-alpha-reductase inhibitors, and anticholinergics.