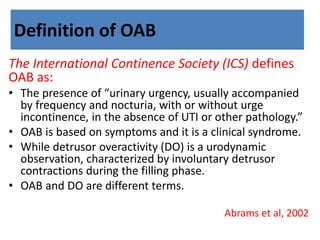
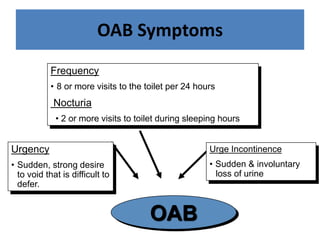
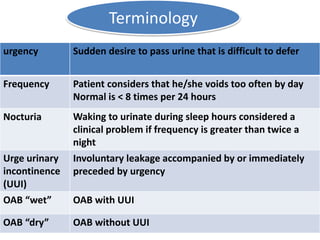
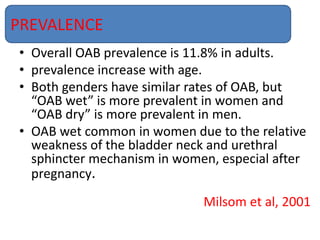
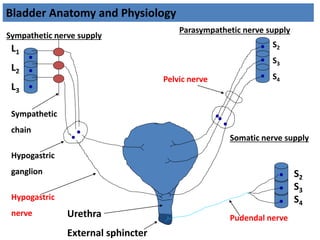
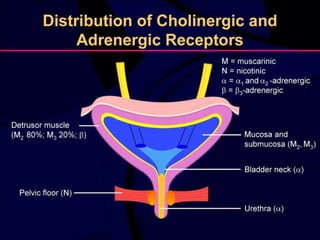
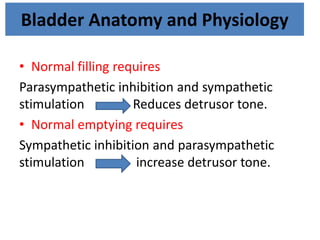
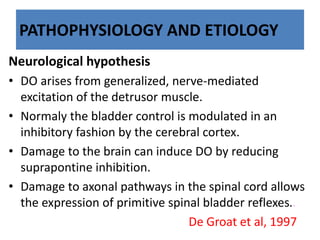
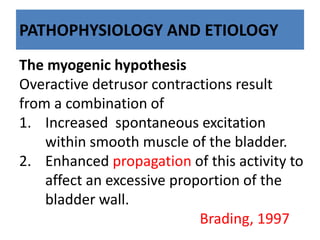
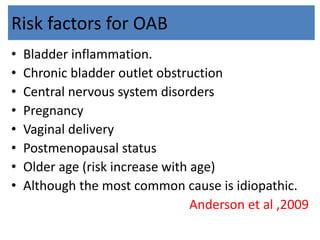
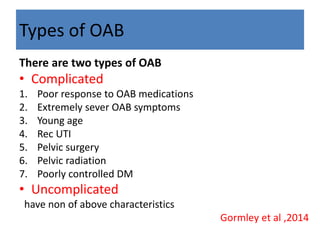
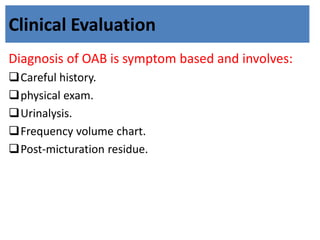
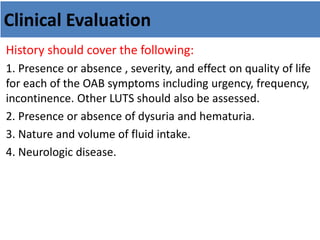
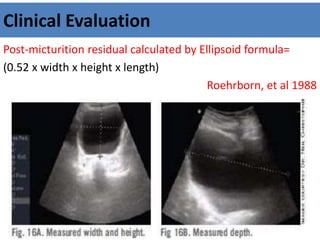
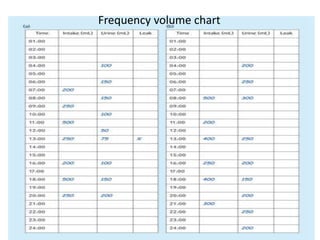
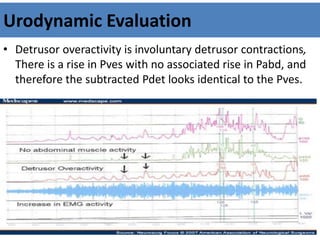
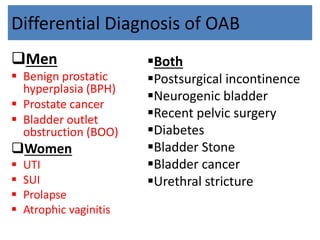
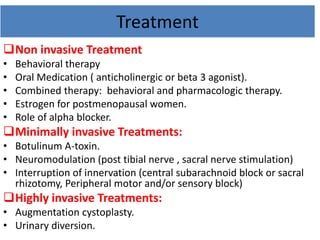
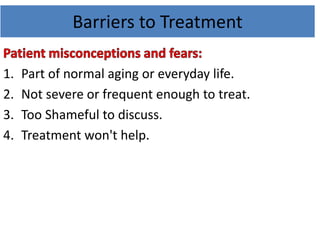
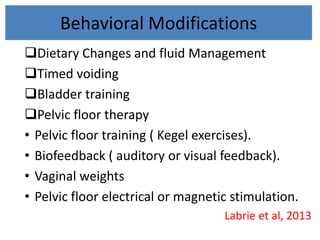
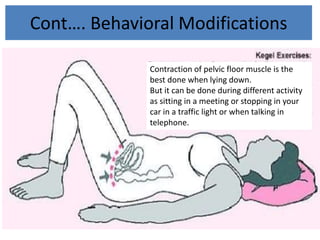
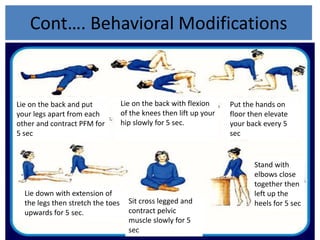
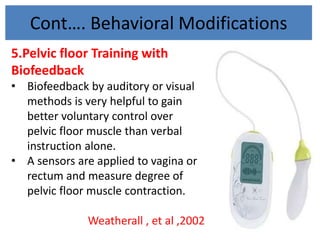
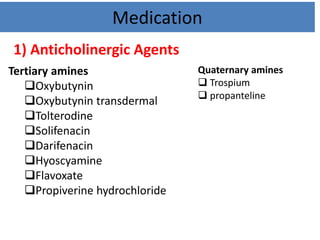
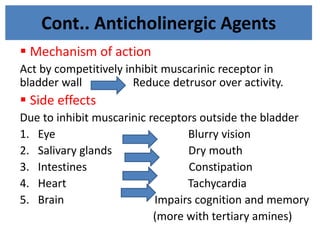
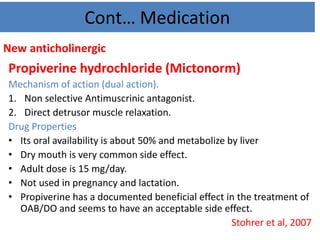
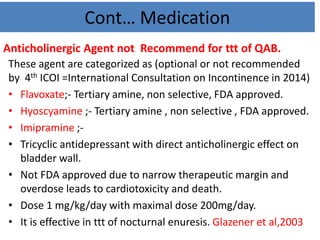
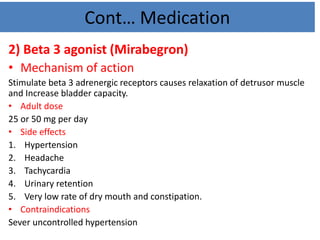
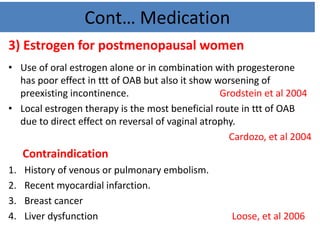
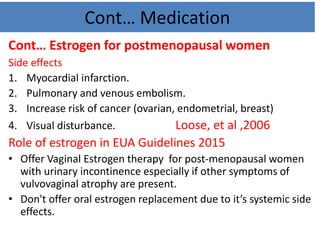
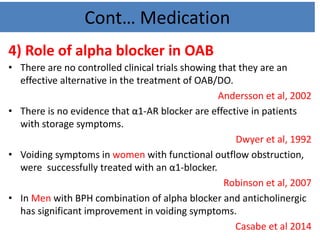
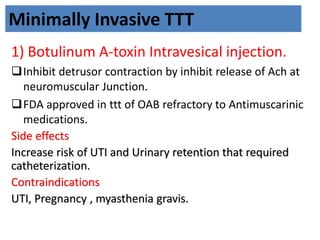
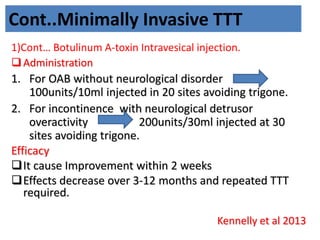
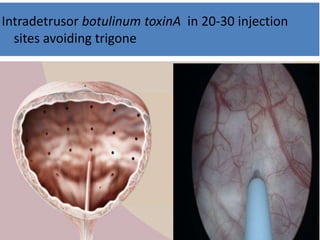
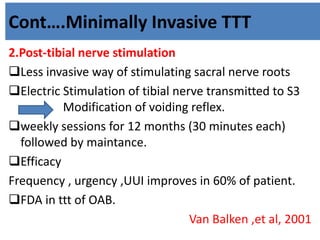
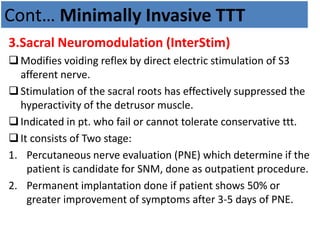
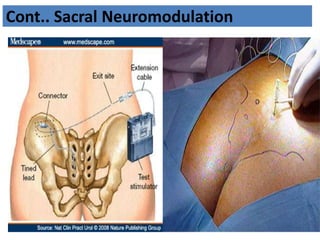
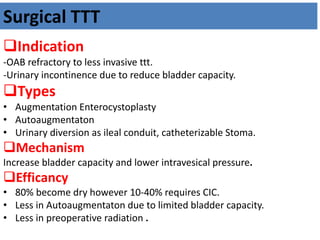
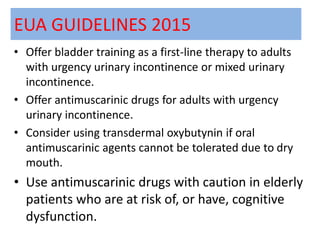
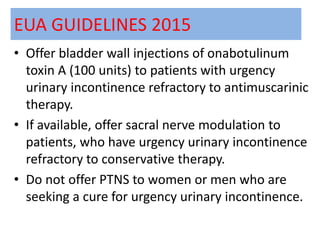
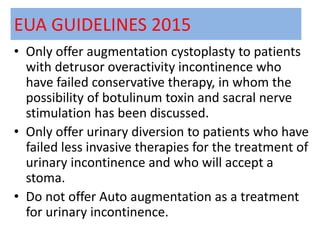
This document provides an overview of overactive bladder (OAB). It defines OAB and its main symptoms of urgency, frequency, and nocturia. It discusses the prevalence of OAB increasing with age and being similar between genders. The document outlines the bladder anatomy and physiology, as well as theories around the etiology and pathophysiology of OAB. It describes the diagnosis and clinical evaluation of OAB through medical history, physical exam, urinalysis, and other tests. Finally, it covers treatment approaches for OAB including behavioral modifications, medications, injections, and surgeries.