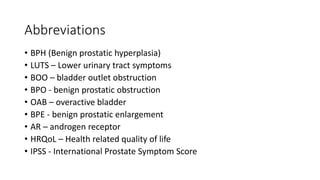
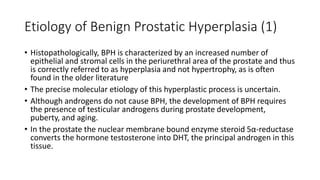
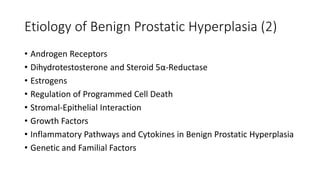
This document provides an overview of benign prostatic hyperplasia (BPH). It defines key terms related to BPH and lower urinary tract symptoms. It describes the histopathology and molecular etiology of BPH, risk factors such as aging and genetics, and the pathophysiology whereby BPH causes bladder outlet obstruction and changes in bladder function. It also discusses complications of BPH, correlations with severity measures, and a staging system for determining appropriate treatment.