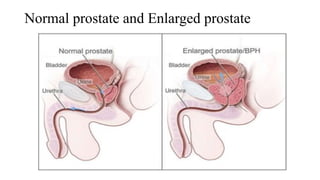
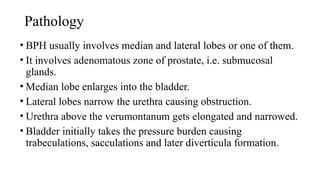
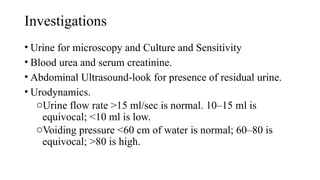
The document provides an overview of benign prostatic hyperplasia (BPH) and urethral stricture, detailing definitions, clinical features, causes, differential diagnoses, and treatment options. BPH is characterized by benign enlargement of the prostate occurring typically between ages 60 and 70, while urethral stricture refers to the narrowing of the urethra, often caused by infections or trauma. Treatment modalities for BPH include medical and surgical options, while urethral stricture may require intermittent dilation or surgery.