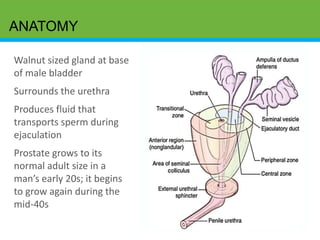
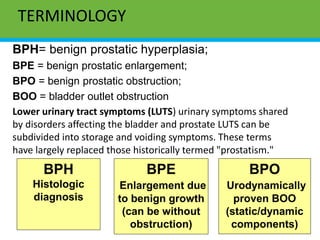
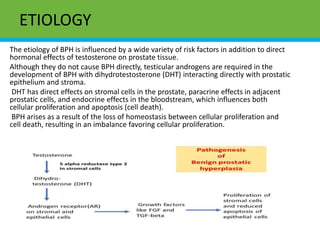
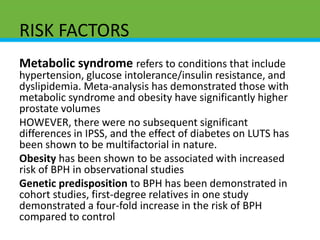
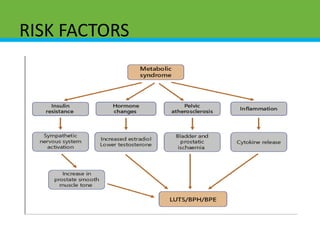
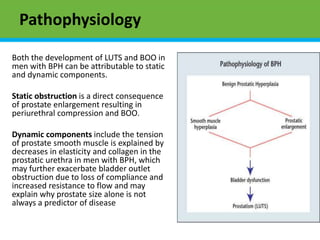
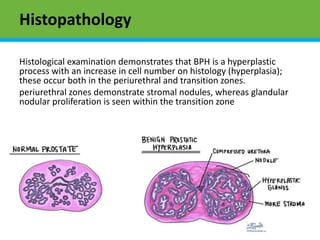
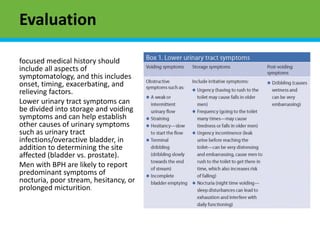
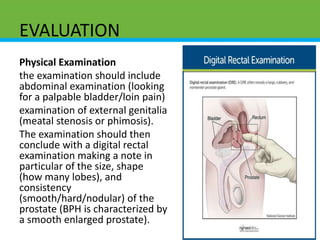
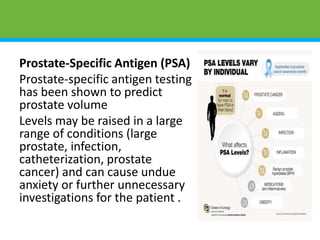
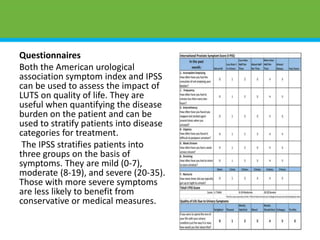
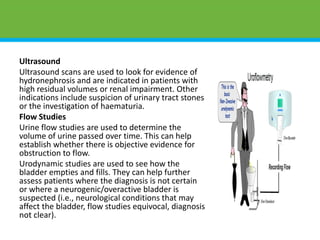
The document summarizes benign prostatic hyperplasia (BPH). It describes the anatomy of the prostate gland and discusses terminology related to BPH. BPH involves benign enlargement of the prostate, which can obstruct the urethra and cause urinary symptoms. Risk factors include increasing age, genetics, and metabolic conditions. Evaluation of BPH involves medical history, physical exam including digital rectal exam, and may include urinalysis, blood tests, questionnaires, ultrasound, and urodynamic studies.