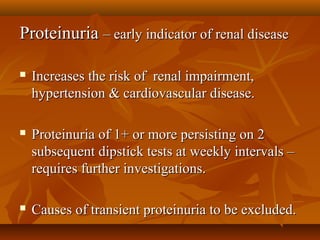
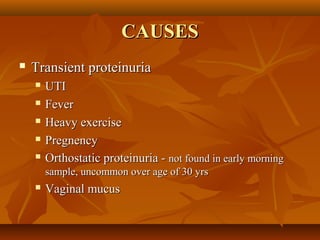
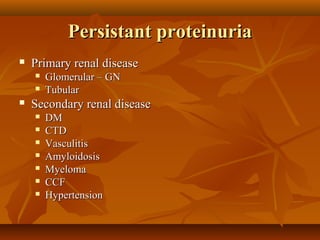
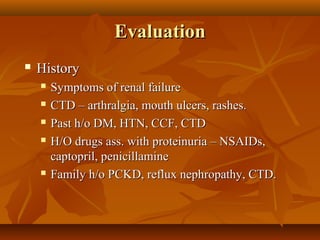
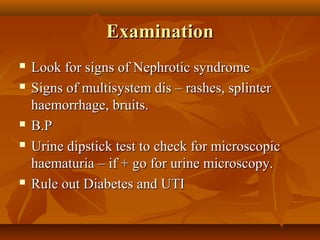
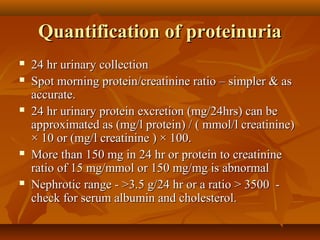
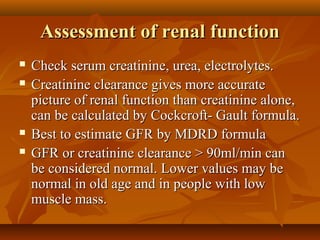
The document discusses proteinuria as an early indicator of renal disease, highlighting its association with renal impairment, hypertension, and cardiovascular disease. It outlines the evaluation process, including causes, assessment of renal function, and quantification of proteinuria, emphasizing the importance of additional investigations and follow-up. Key points include identifying persistent proteinuria through dipstick tests and managing any associated hypertension with ACE inhibitors or ARBs.