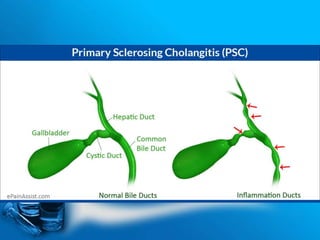
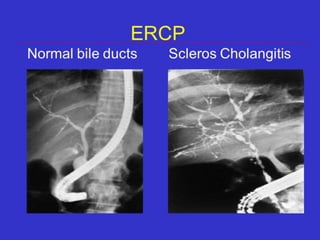
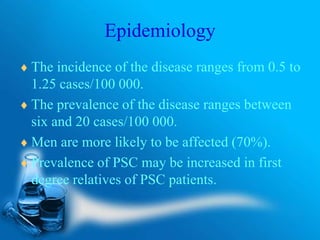
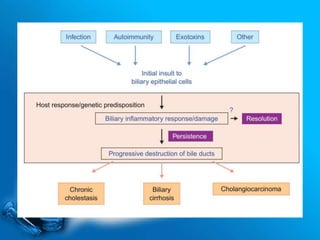
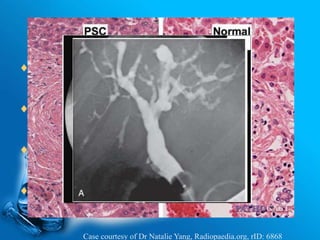
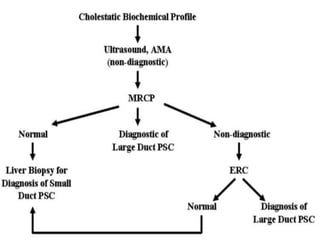
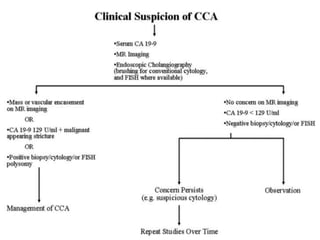
Primary sclerosing cholangitis is a chronic progressive disease characterized by inflammation and fibrosis of the bile ducts. It has unknown causes but likely involves genetic and immunological factors. The disease varies in progression and can result in complications like end-stage liver disease, portal hypertension, cholangitis, or cholangiocarcinoma. While most patients with primary sclerosing cholangitis have inflammatory bowel disease, only a minority of inflammatory bowel disease patients develop primary sclerosing cholangitis. There are no proven effective treatments, so management focuses on supportive care and transplantation may be considered for complications.