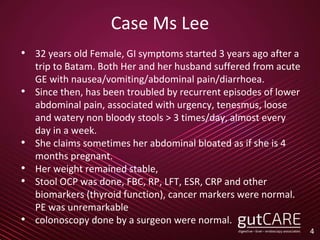
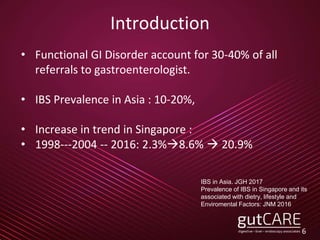
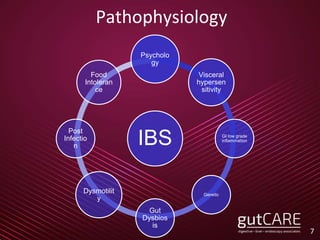
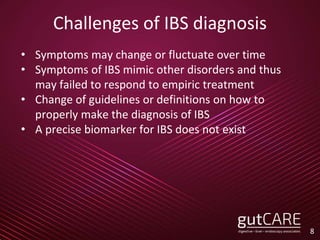
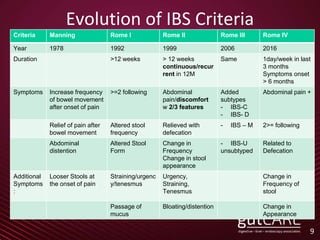
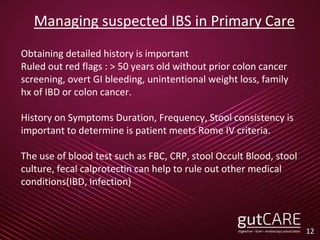
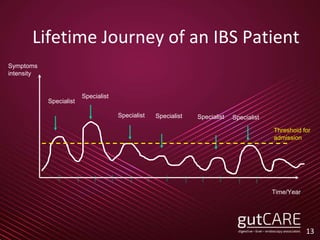
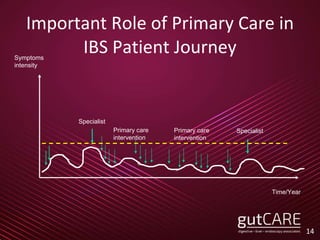
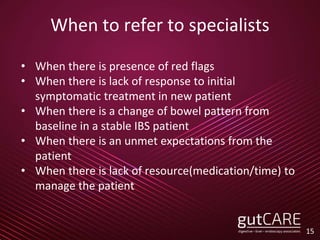
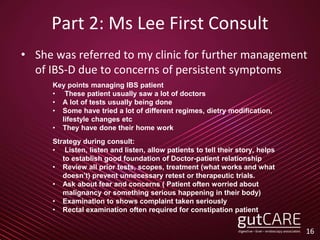
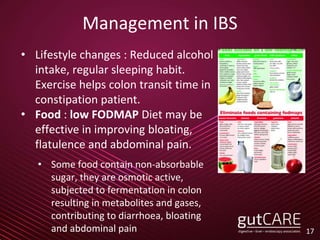
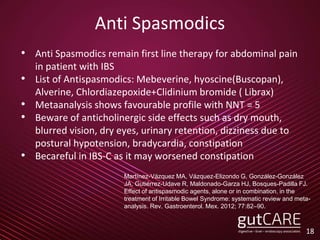
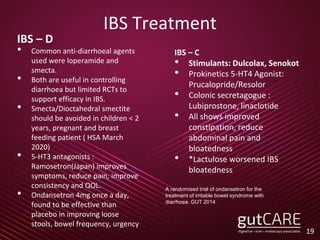
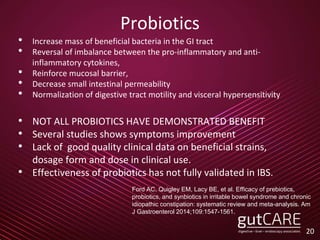
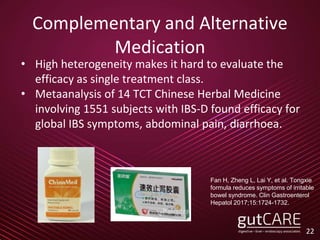
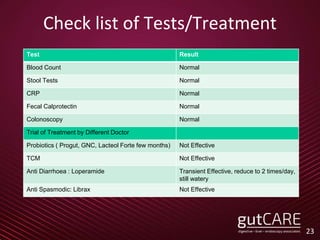
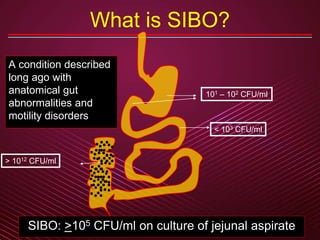
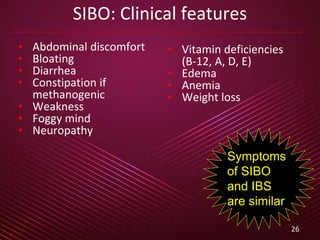
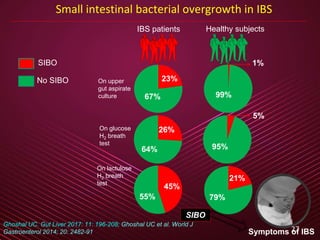
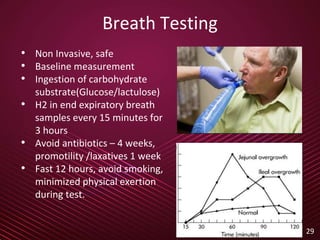
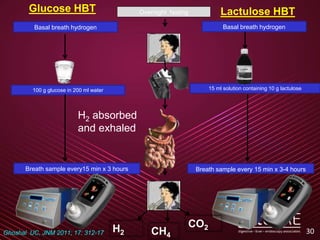
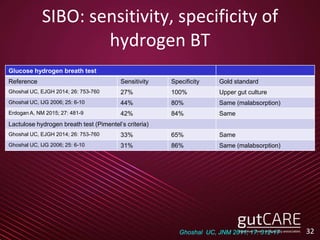
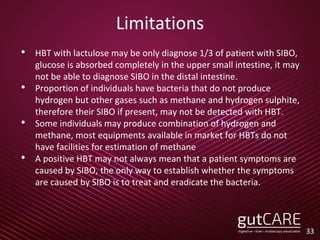
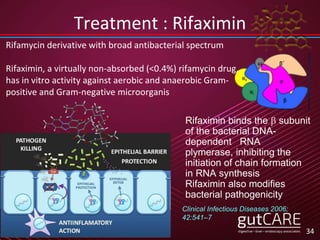
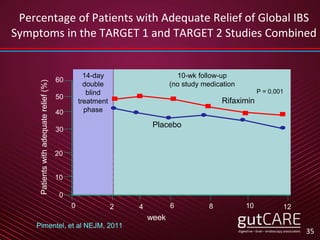
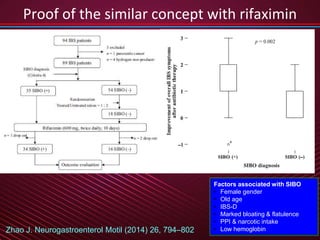
The document presents updates on the understanding and management of irritable bowel syndrome (IBS) in clinical practice, emphasizing the evolving diagnostic criteria from Rome III to Rome IV and the role of small intestinal bacterial overgrowth (SIBO). Key points discussed include treatment options for IBS and the importance of thorough patient assessments to manage persistent symptoms effectively. The document highlights the significant role of primary care in diagnosing and treating IBS, as well as the potential benefits of rifaximin in addressing SIBO-related symptoms.