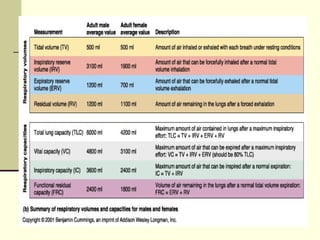
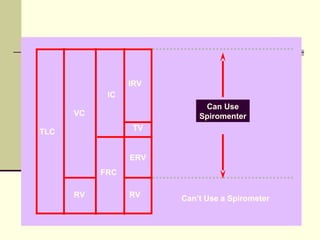
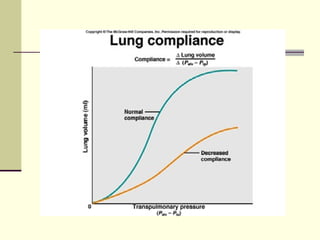
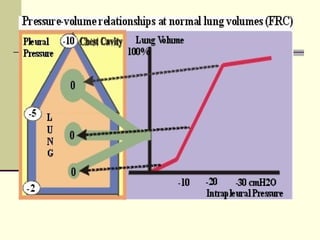
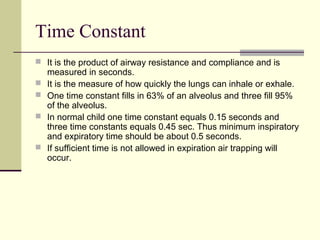
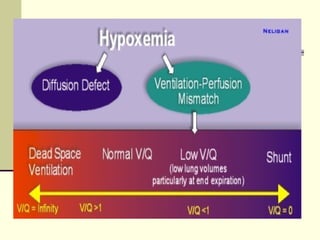
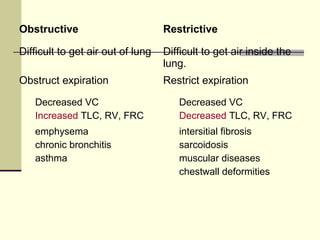
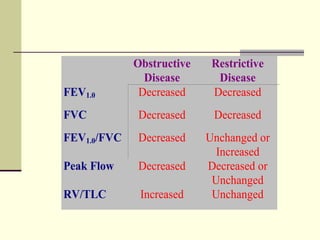
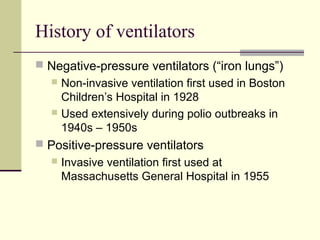
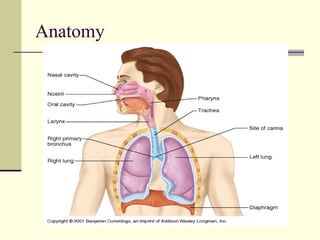
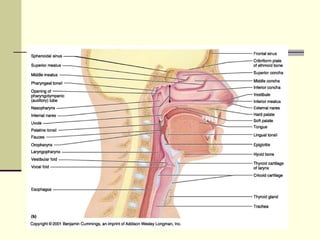
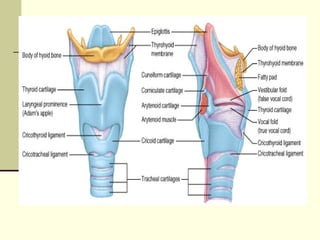
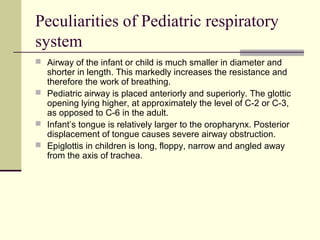
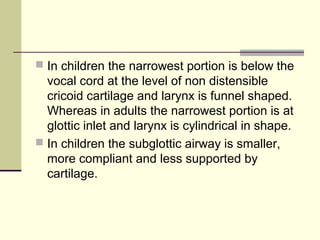
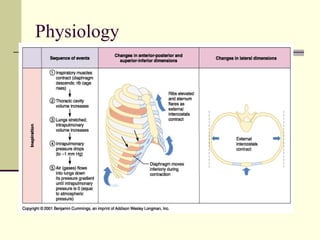
This document discusses pediatric ventilation basics including anatomy, physiology, pathophysiology, and terminology. Key points include: the pediatric airway is smaller and more anteriorly placed; children have higher oxygen needs and lower tolerance for hypoxia; compliance is lower in children; and ventilator settings like tidal volume, rate, inspiratory time, and PEEP must be adjusted for pediatric patients. Common pediatric lung conditions and how they impact pulmonary function tests and the ventilation/perfusion ratio are also reviewed.
![Alveolar Gas Equation
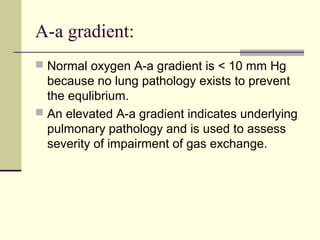
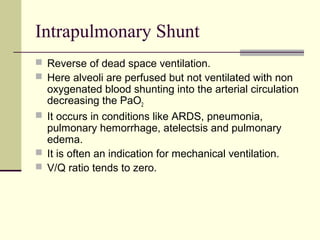
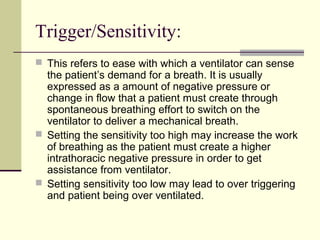
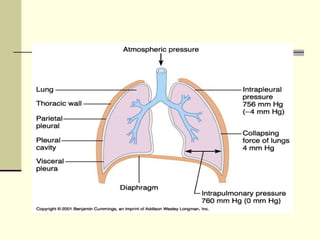
PAO2 is calculated by the alveolar gas equation:
PAO2= [FiO2(Pb-PH2O)]-(Paco2/R)
FiO2 = Fraction of the inspired oxygen
e.g. Breathing oxygen at room air with conc 21% FiO2=0.21
Pb is the barometric pressure ( assumed to be 760 mm Hg at sea
level.
PH2O= Water vapor pressure which dilutes dry oxygen content of
the atmosphere= 47 mm Hg.
R= respiratory quotient assumed to be 0.8
Thus PAO2 depends on FiO2 i.e. fraction of the inspired oxygen.
More the FiO2 ,higher will be the PAO2.](https://image.slidesharecdn.com/basicsofpediatricventilation-150109001512-conversion-gate01/85/Basics-of-pediatric-ventilation-14-320.jpg)