The document discusses mechanical ventilation, including:
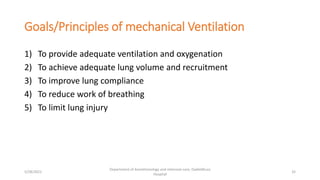
1) The objectives of discussing the basic physiology and physics of the lung and ventilator, different modes of mechanical ventilation, troubleshooting, and weaning.
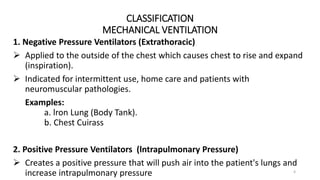
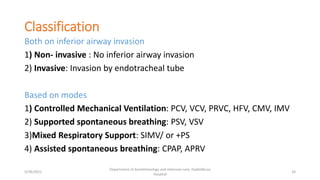
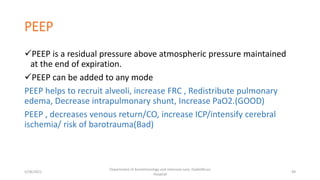
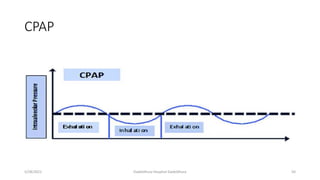
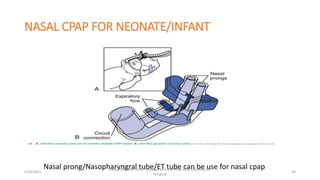
2) Classifying mechanical ventilation based on airway pressure (negative vs positive pressure) and invasiveness (invasive vs non-invasive).
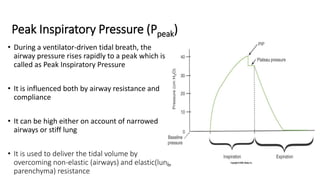
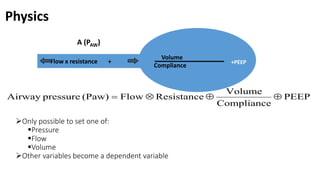
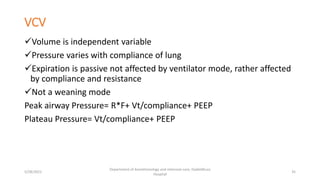
3) Explaining volume-controlled ventilation where volume is the independent variable and pressure varies with lung compliance. Expiration is passive and not affected by the ventilator mode.