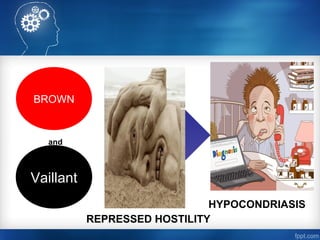
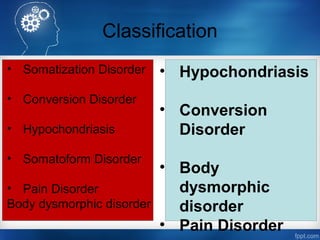
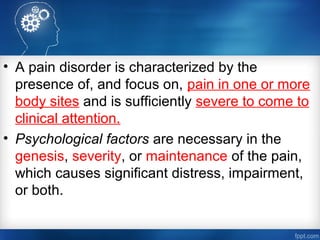
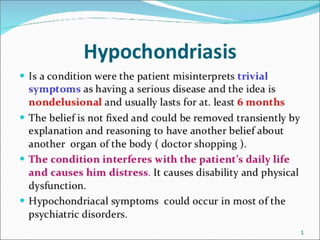
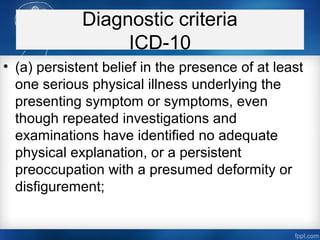
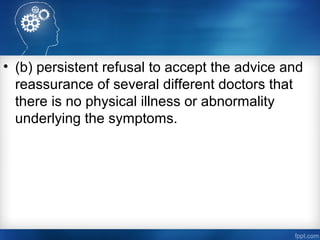
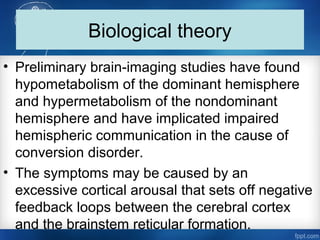
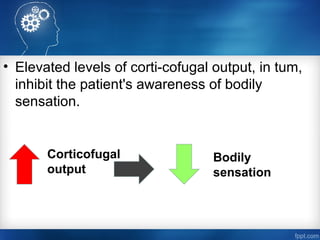
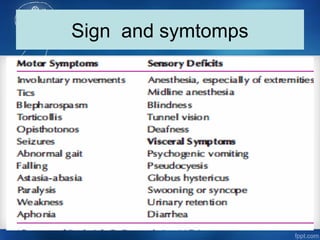
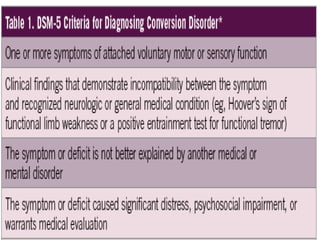
Somatoform disorders are psychological conditions characterized by physical symptoms with no identifiable medical cause, historically viewed as due to spiritual possession. Current understanding attributes these symptoms to various psychological and behavioral factors, which may include coping mechanisms for emotional distress. Management typically involves a combination of pharmacotherapy, behavioral interventions, and supportive psychotherapy to address both the physical complaints and underlying psychological issues.