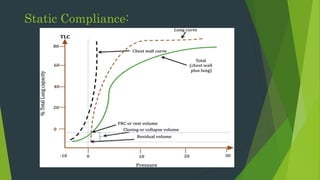
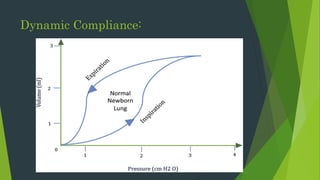
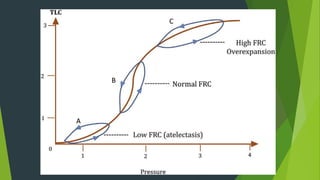
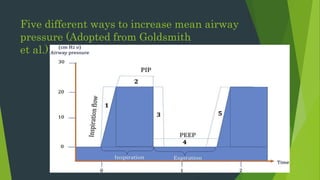
The document discusses the basics of neonatal mechanical ventilation, focusing on its goals to oxygenate infants while minimizing lung damage. It covers key aspects such as the mechanics of breathing, lung compliance, resistance, and the importance of adjustments in ventilation settings to optimize gas exchange. A thorough understanding of neonatal lung physiology is emphasized for effective respiratory support and decision-making in clinical practice.