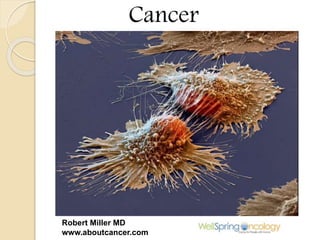
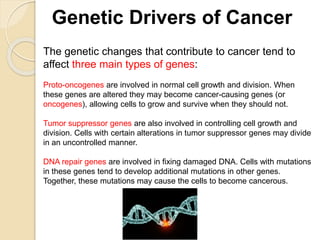
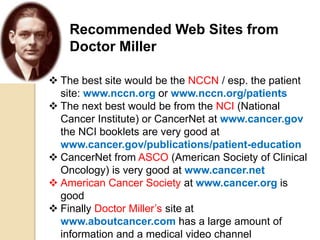
Cancer is a collection of related diseases characterized by uncontrolled cell division and can be caused by genetic changes. The document outlines various cancer types, staging systems, and important factors that influence prognosis, including genetics and treatment options. It emphasizes the importance of a multidisciplinary approach in decision-making for the best patient outcomes.