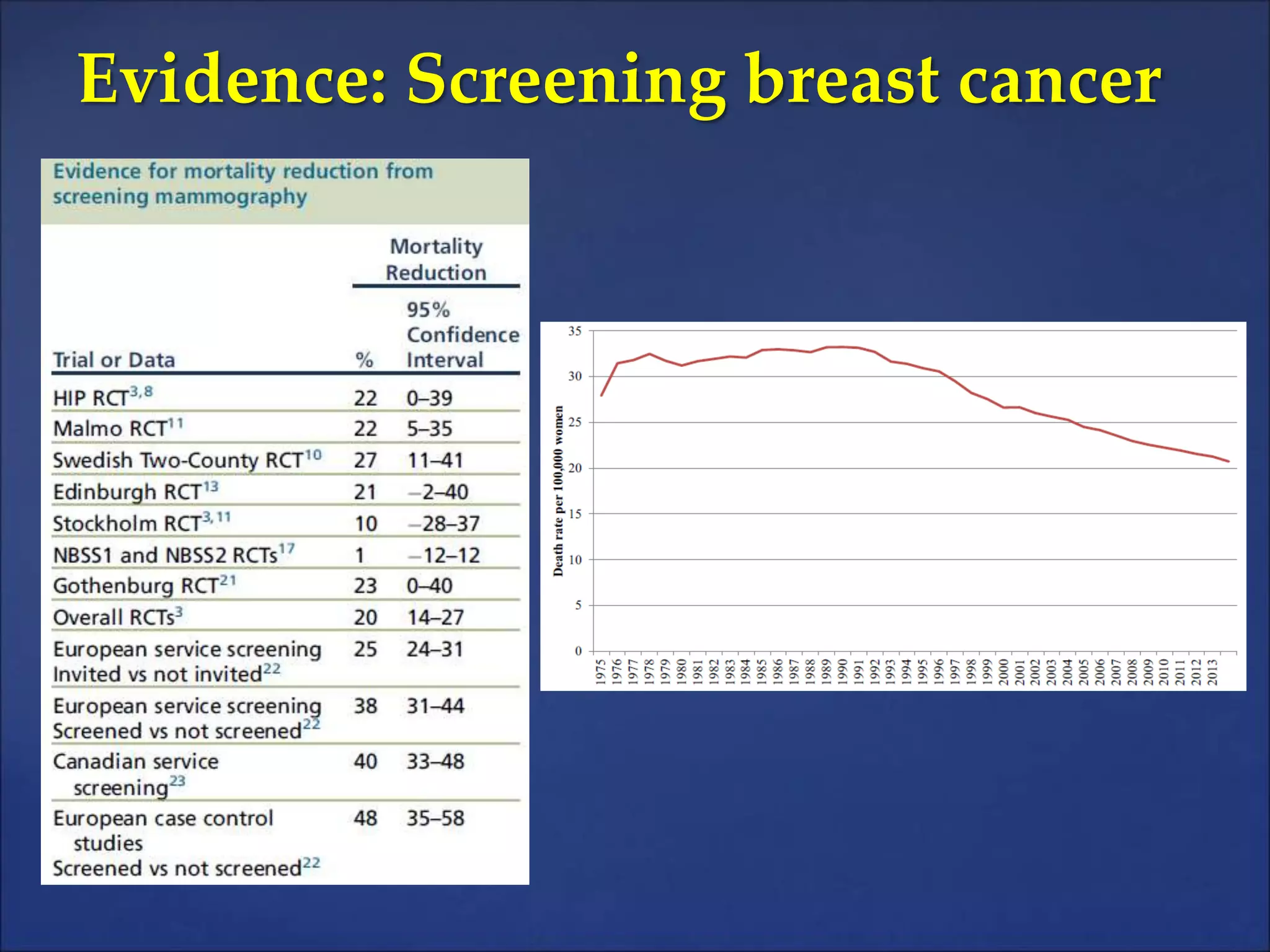
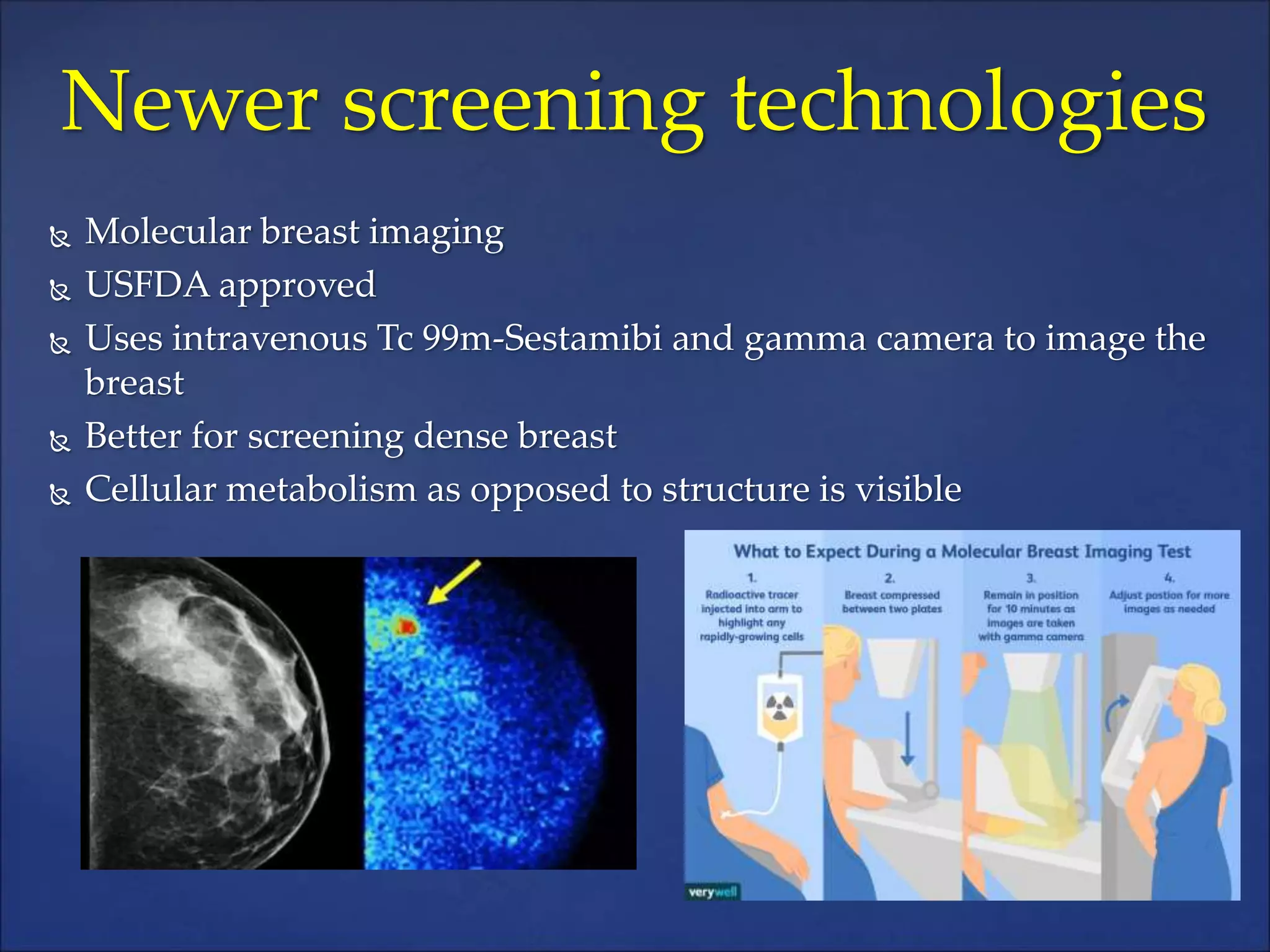
Dr. Ajeet Kumar Gandhi discusses breast cancer screening in India, highlighting its high incidence and mortality rates among women. He outlines the effectiveness of screening technologies like mammography, tomosynthesis, and MRI, as well as emerging techniques, emphasizing the importance of tailored screening for high-risk individuals. The document also addresses the risks of screening processes, including false positives and the psychological impact on patients, while advocating for informed discussions with patients regarding the benefits and limitations of screening.