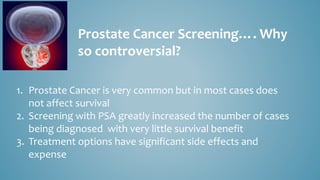
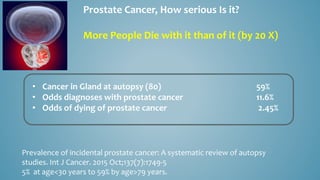
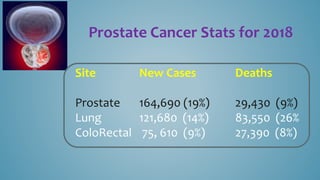
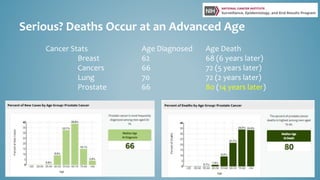
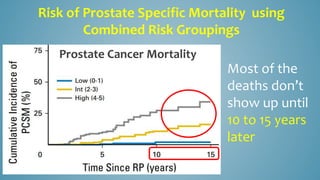
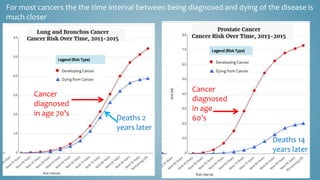
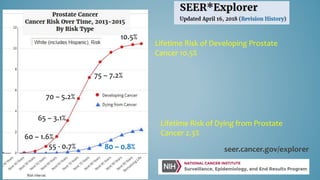
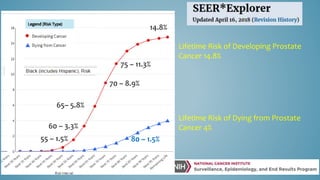
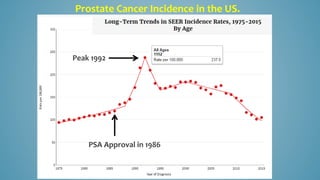
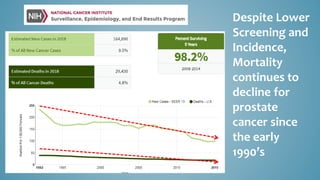
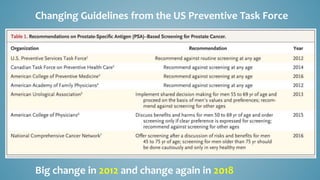
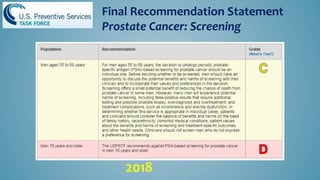
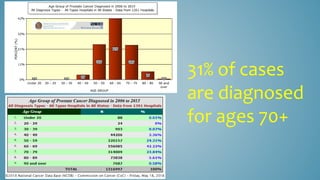
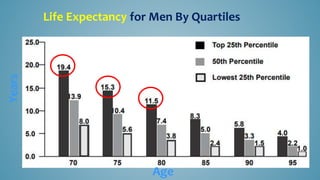
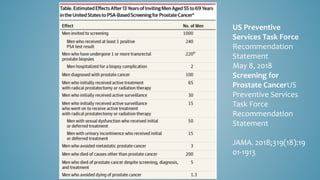
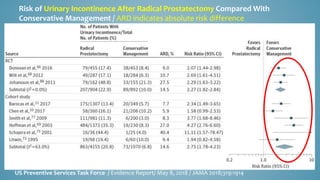
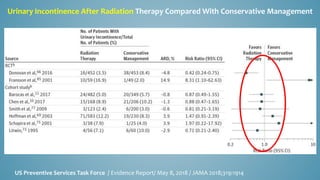
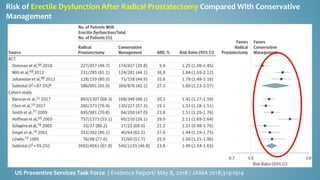
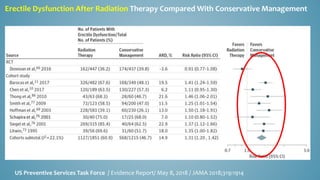
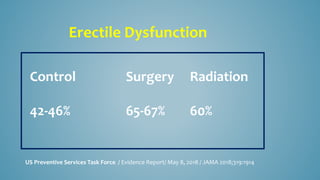
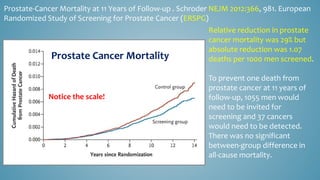
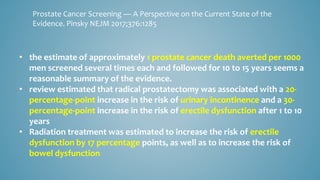
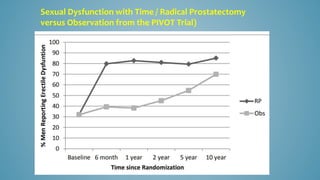
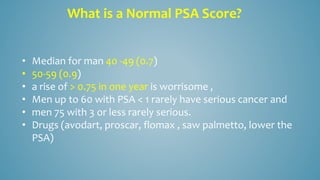
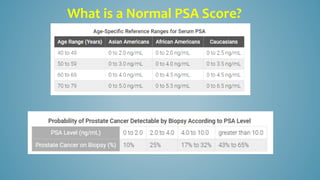
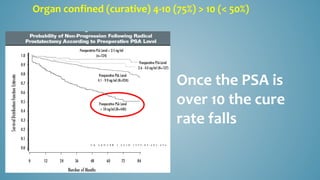
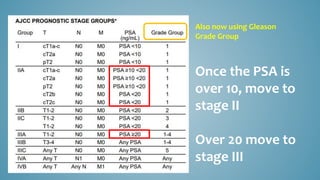
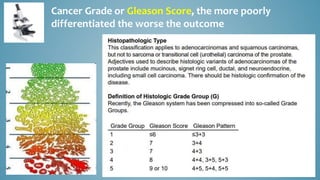
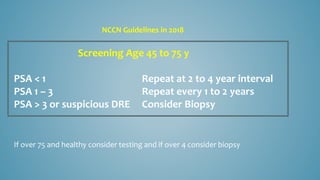
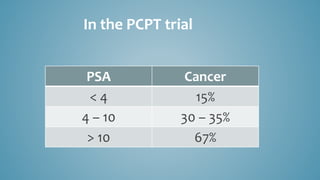
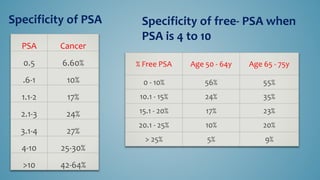
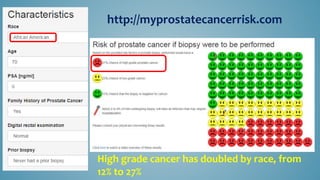
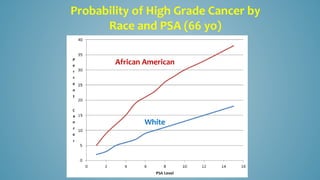
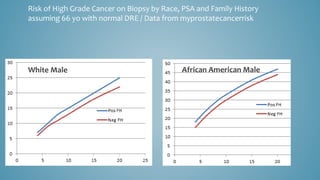
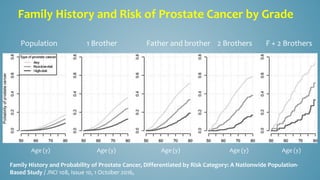
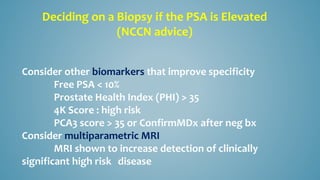
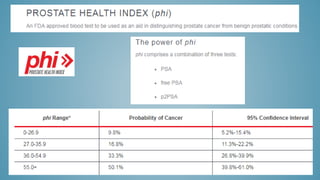
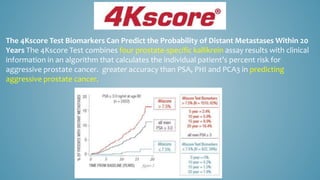
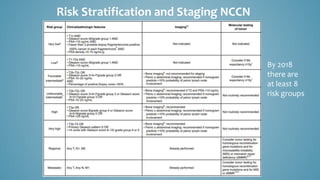
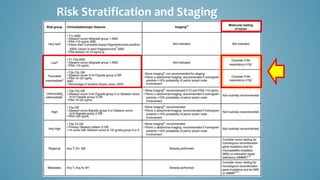
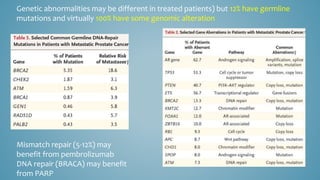
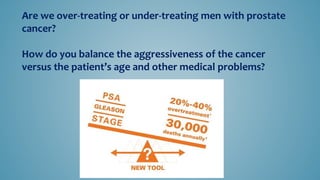
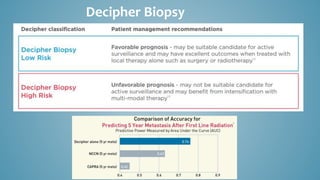
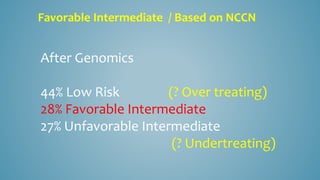
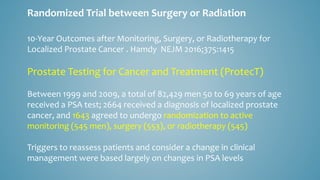
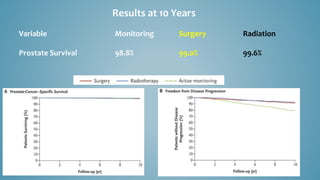
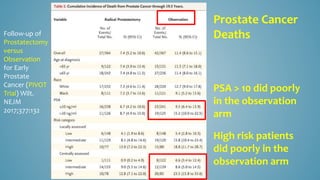
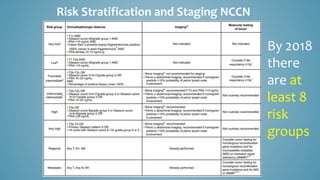
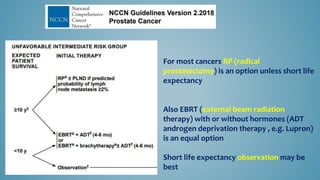
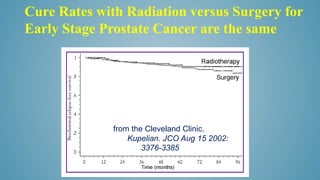
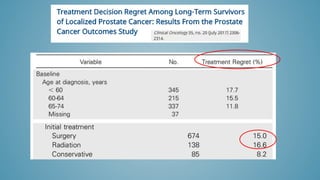
Prostate cancer screening is controversial due to high diagnosis rates but minimal survival benefits, coupled with significant treatment side effects and costs. Most men die with prostate cancer rather than from it, with varying lifetime risks of developing and dying from the disease. New guidelines stress careful screening and treatment decision-making, emphasizing emerging roles of MRI, genomics, and individualized risk stratification.