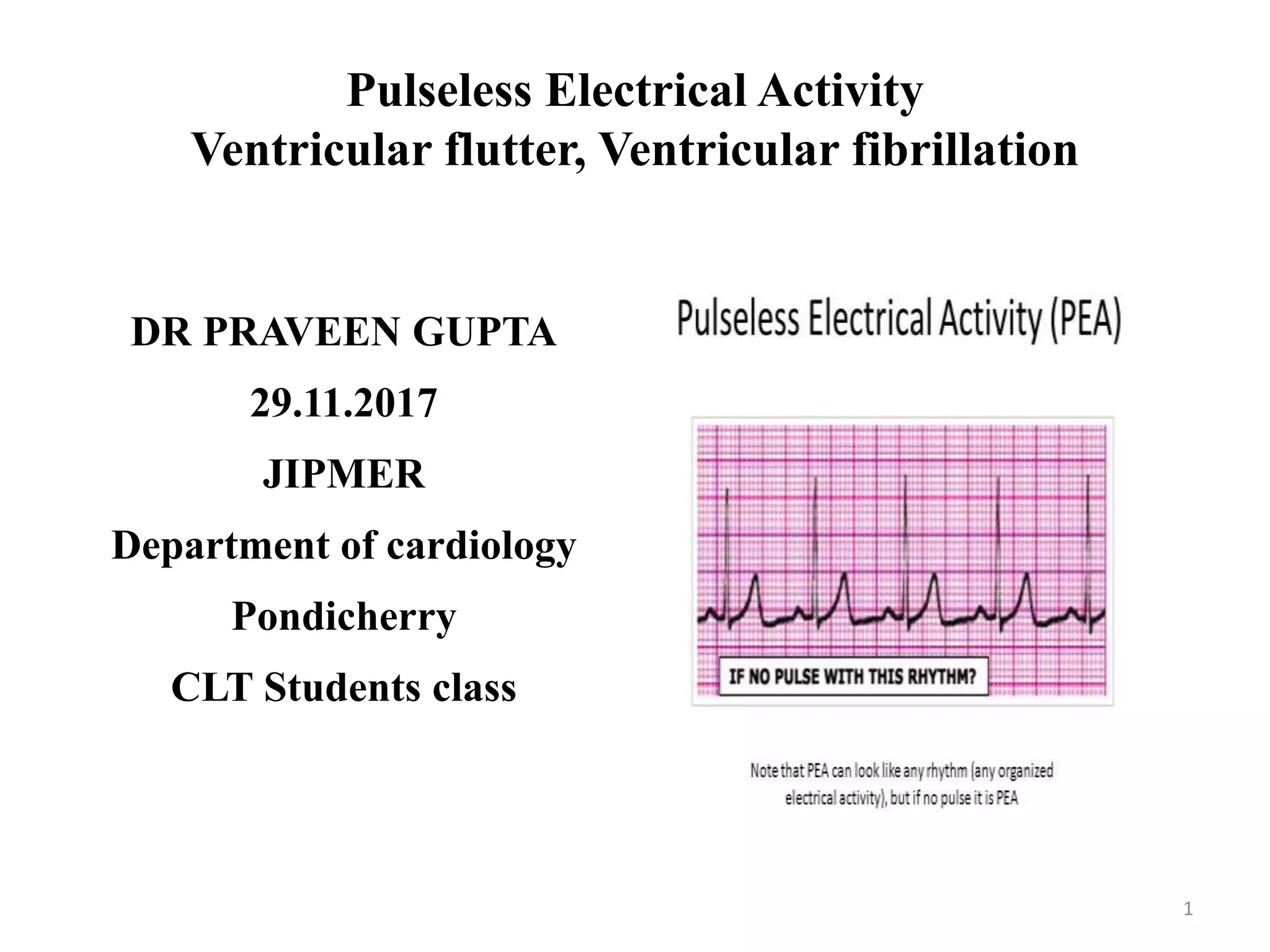
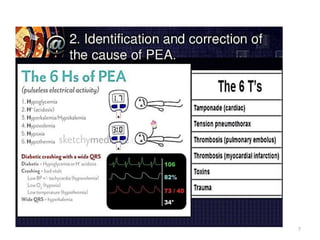
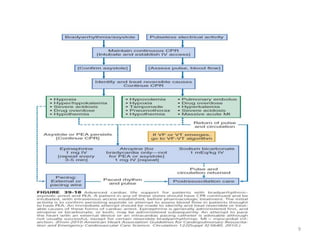
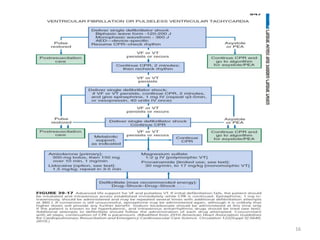
1) Pulseless electrical activity (PEA) occurs when organized cardiac electrical activity is present but fails to produce adequate mechanical activity and blood flow. 2) Causes of PEA include hypoxia, acidosis, decreased contractility, and increased afterload. 3) Ventricular flutter and fibrillation represent severe irregularities of the heartbeat that can quickly lead to loss of consciousness and death if not treated with defibrillation.