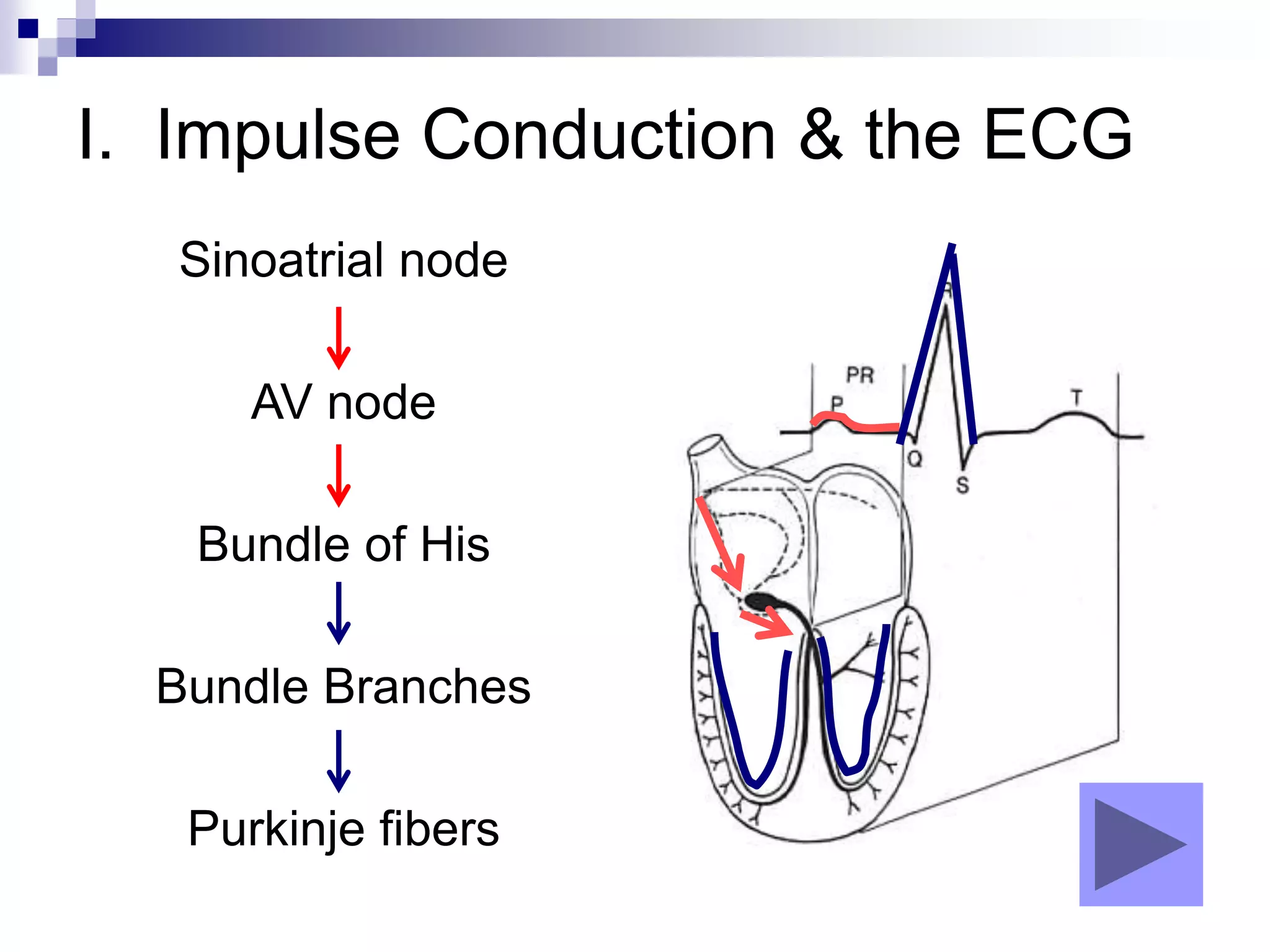
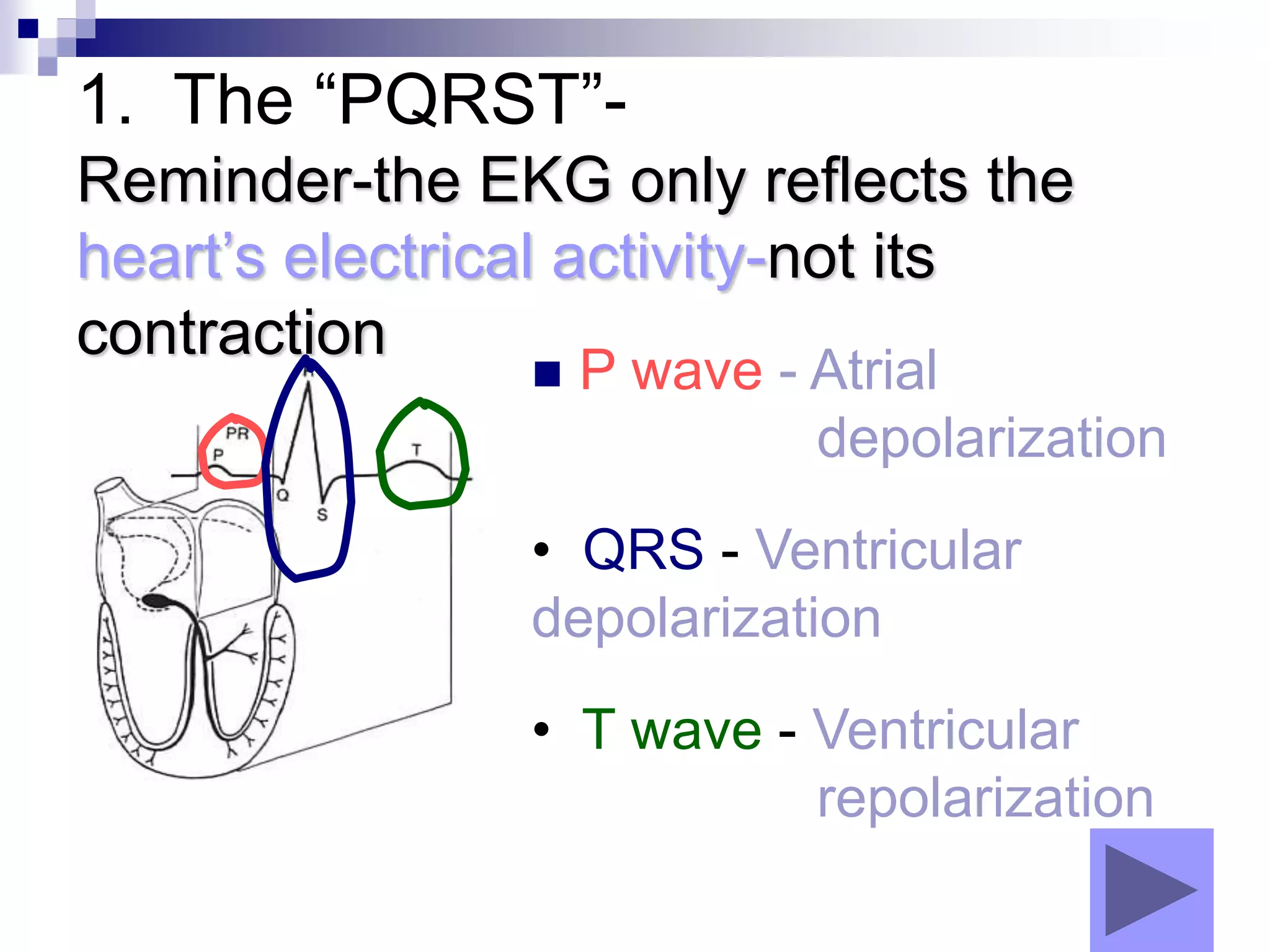
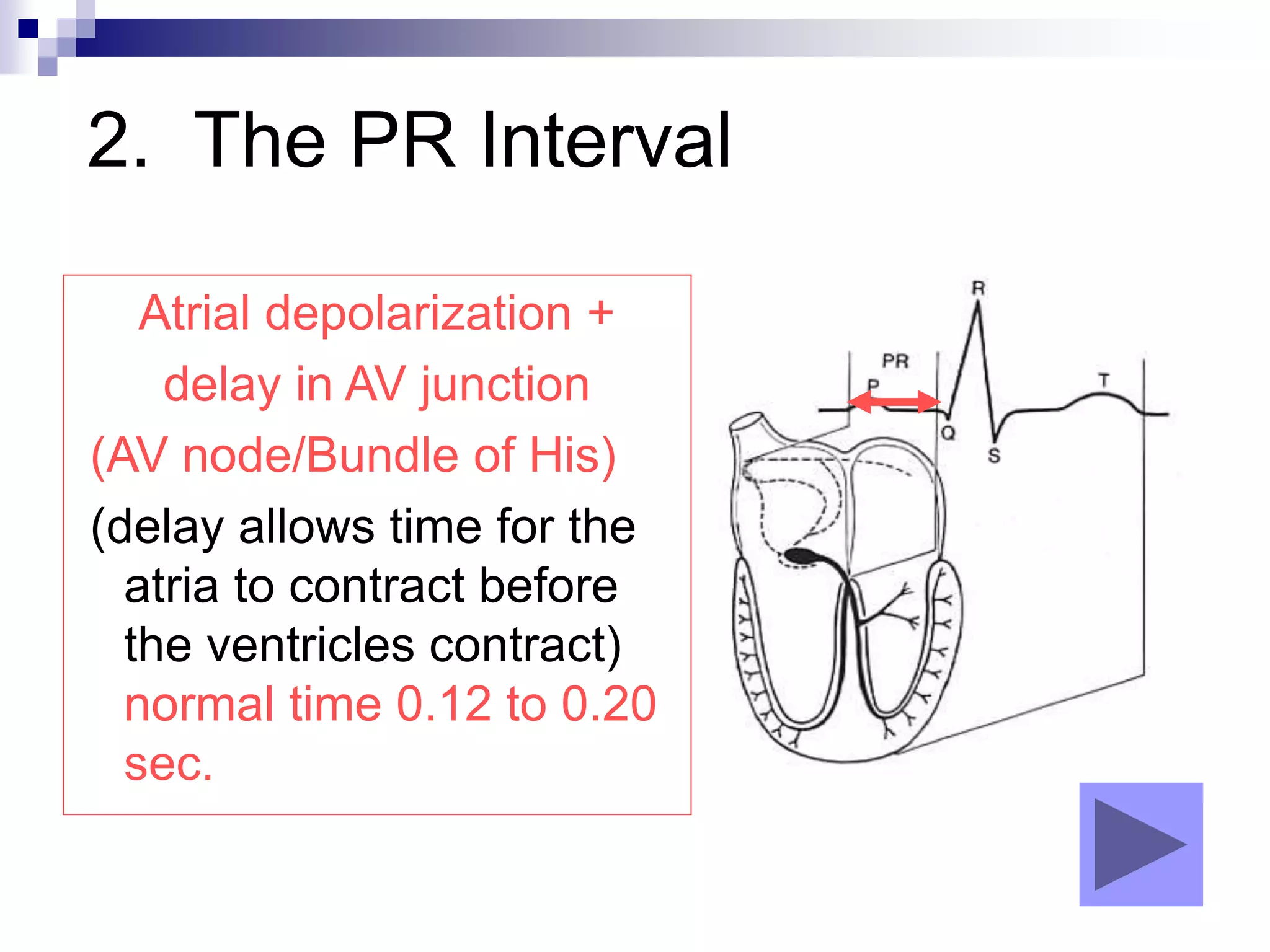
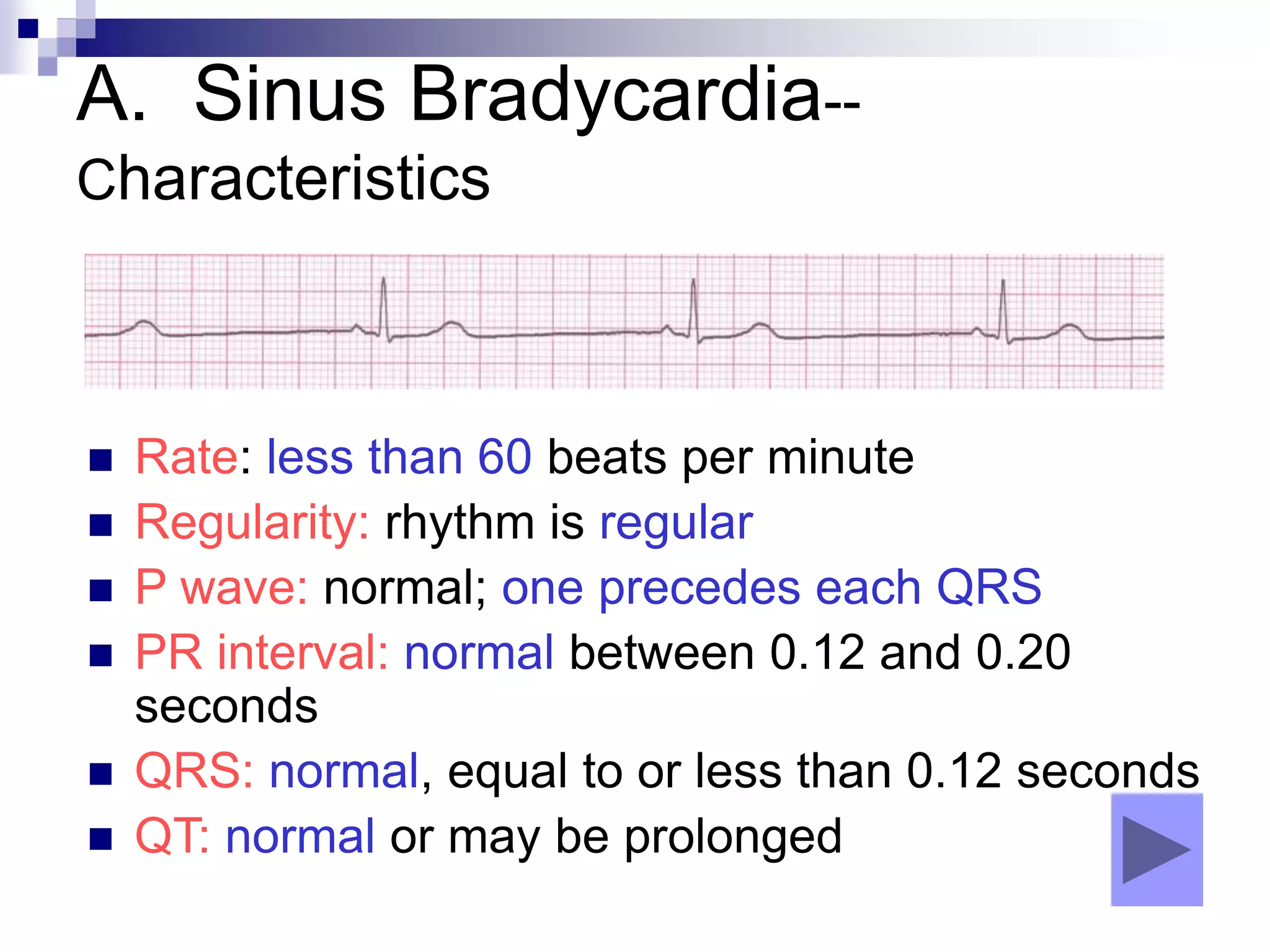
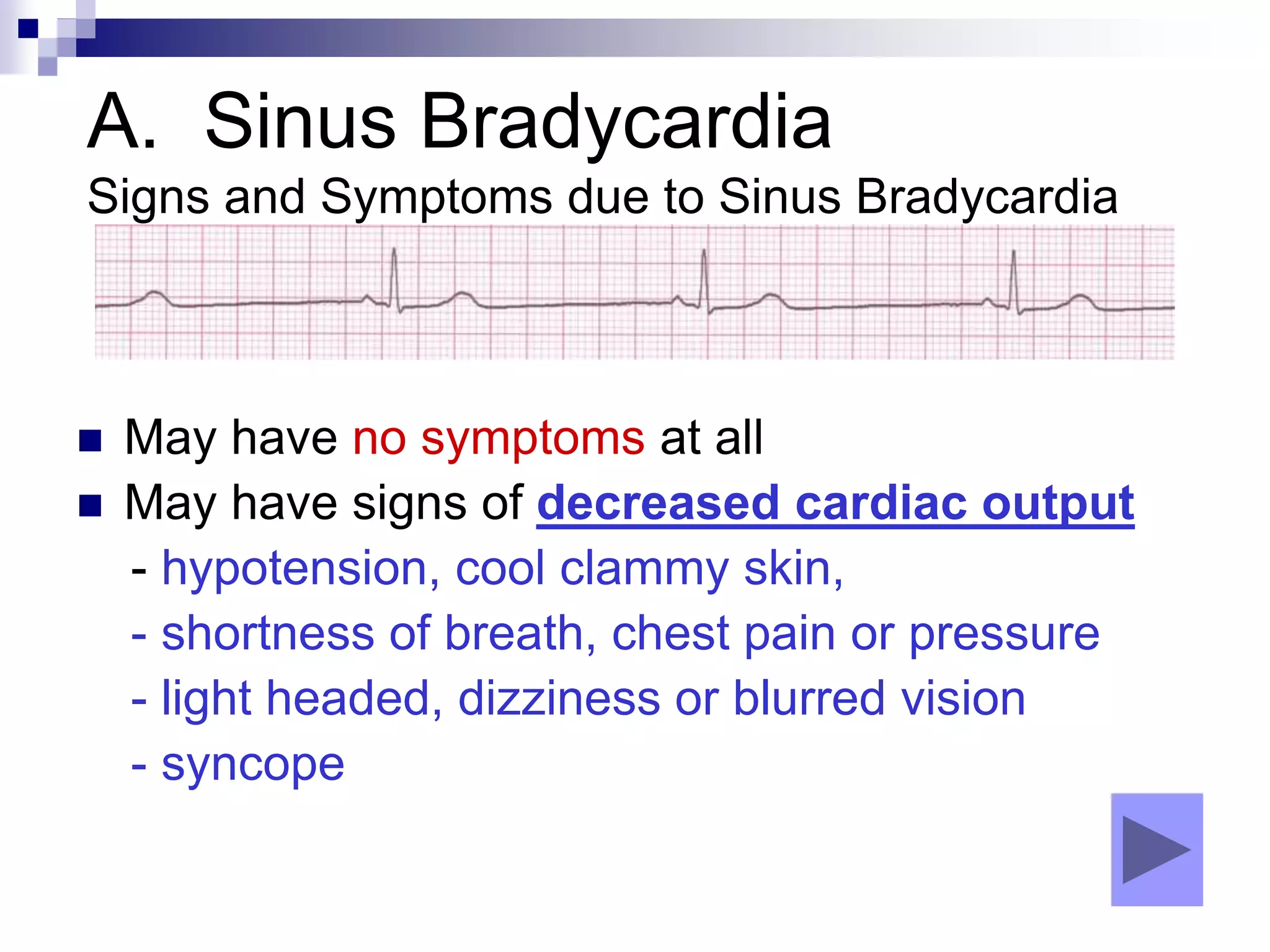
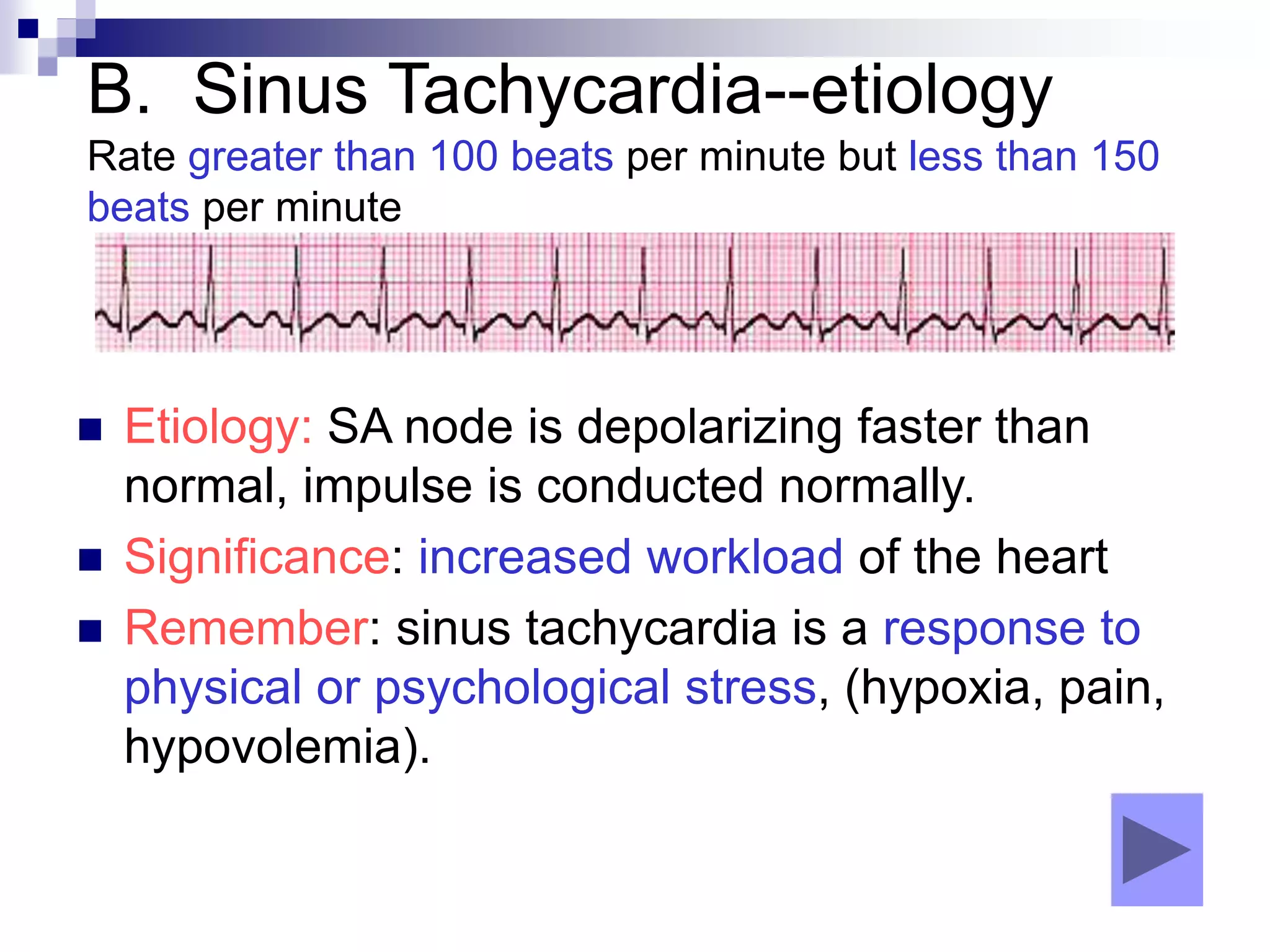
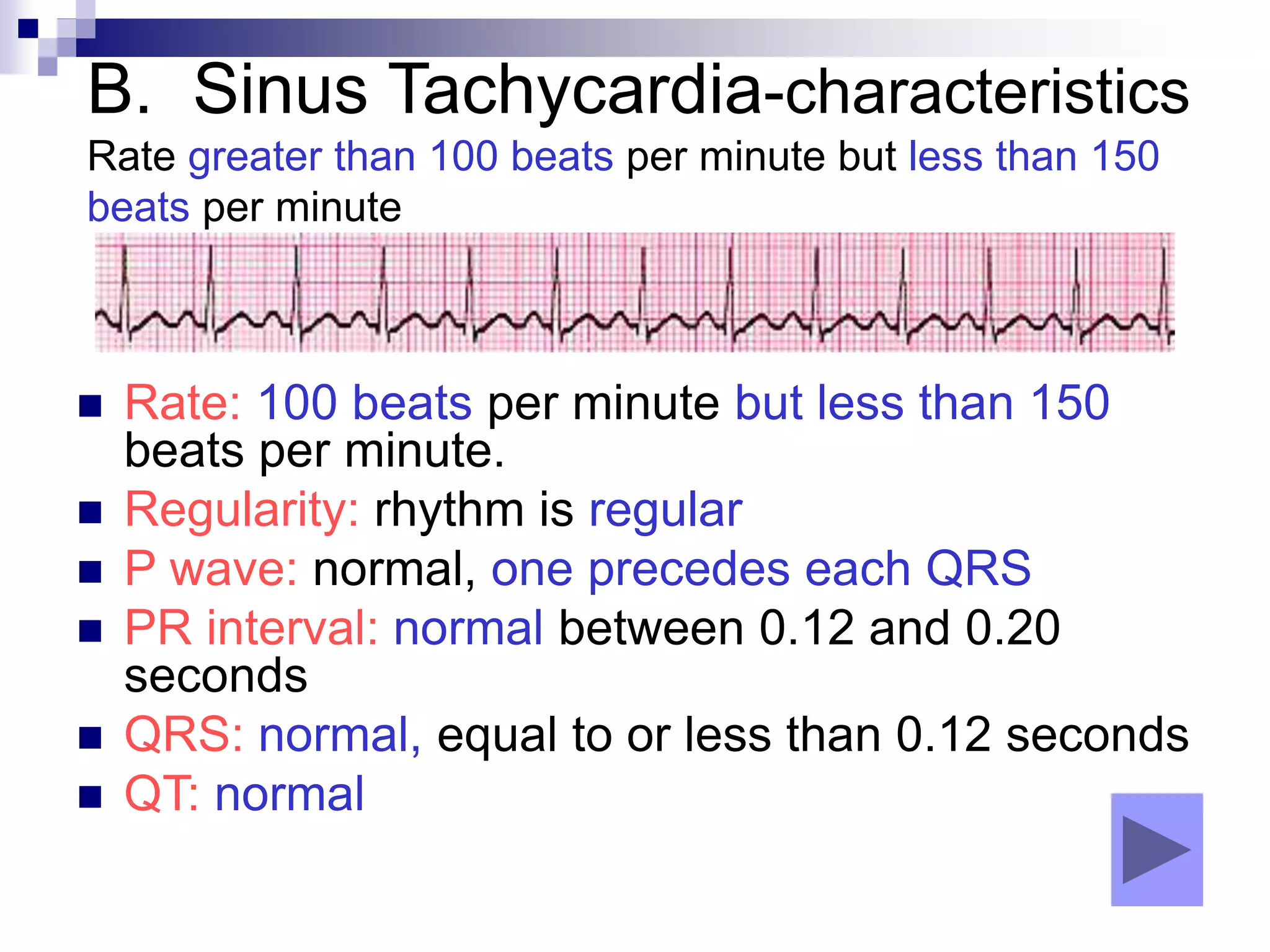
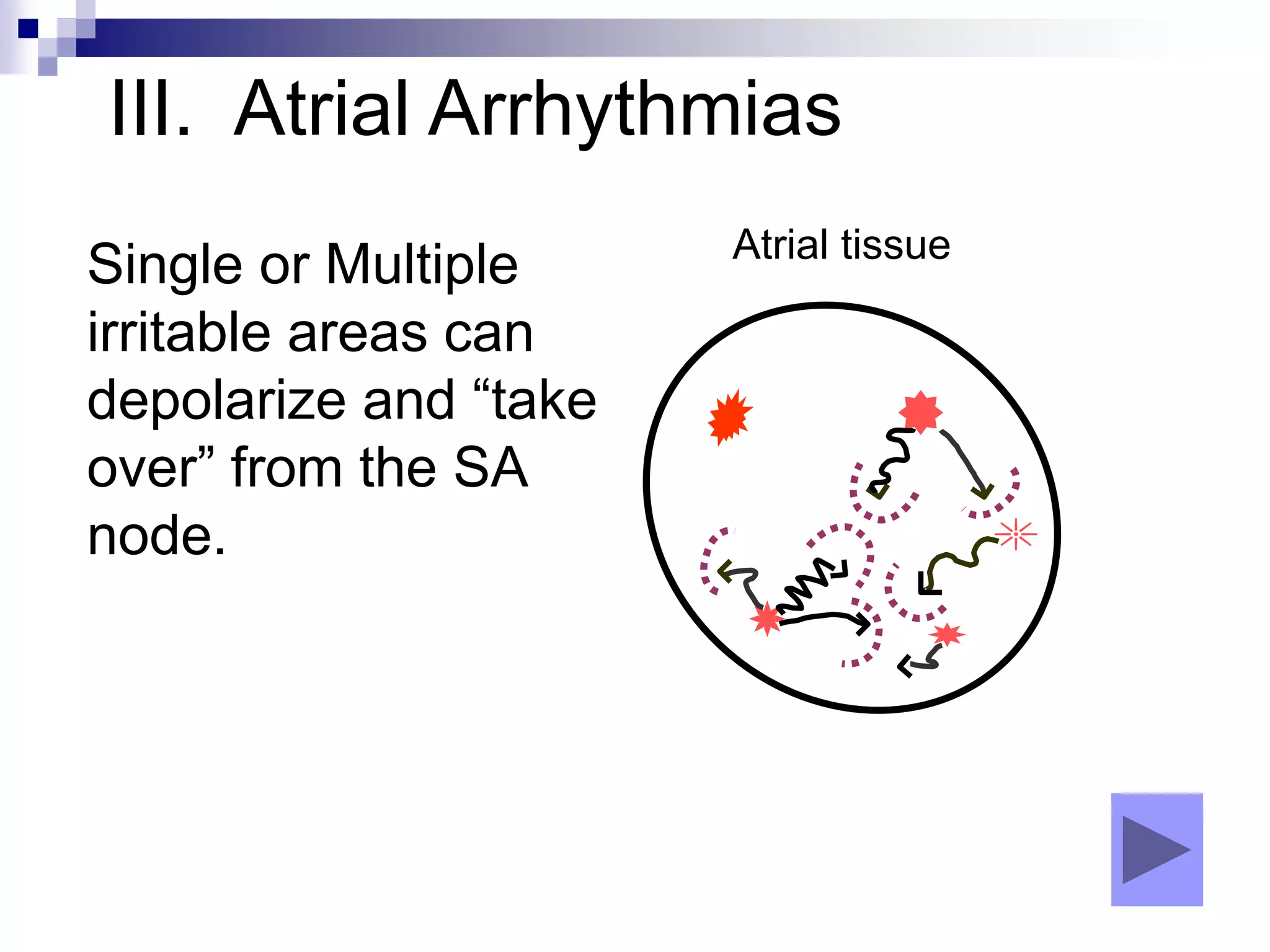
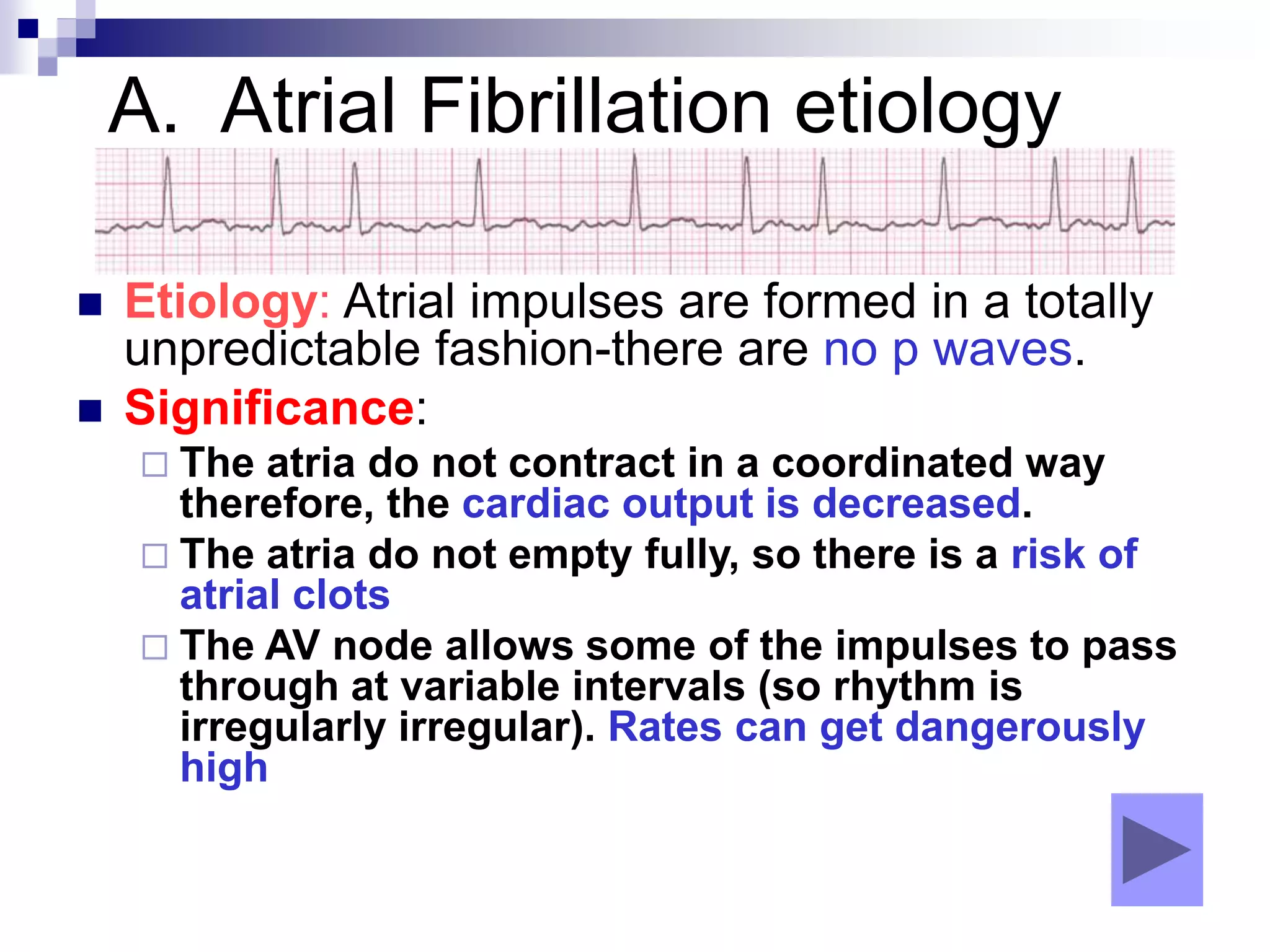
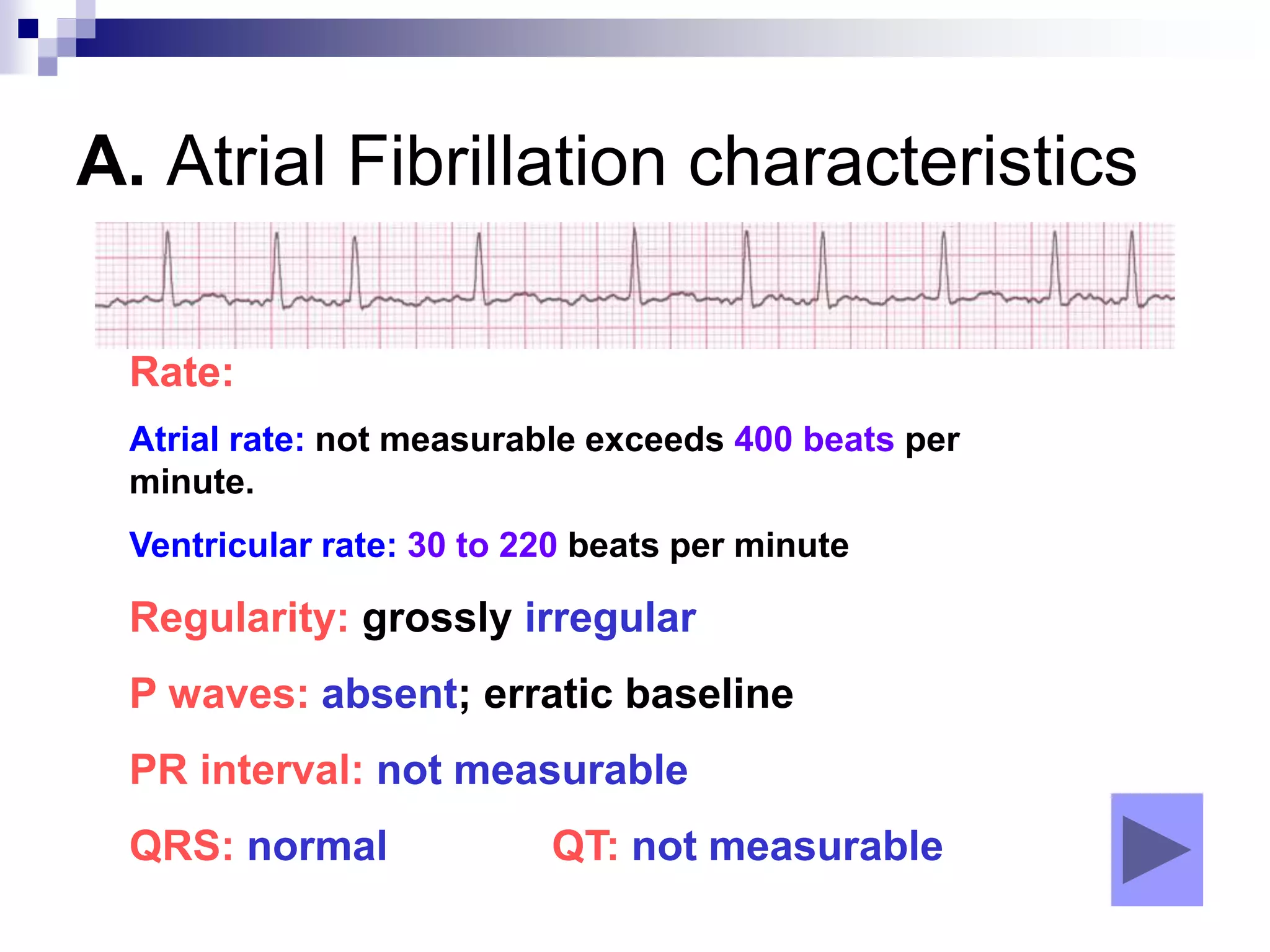
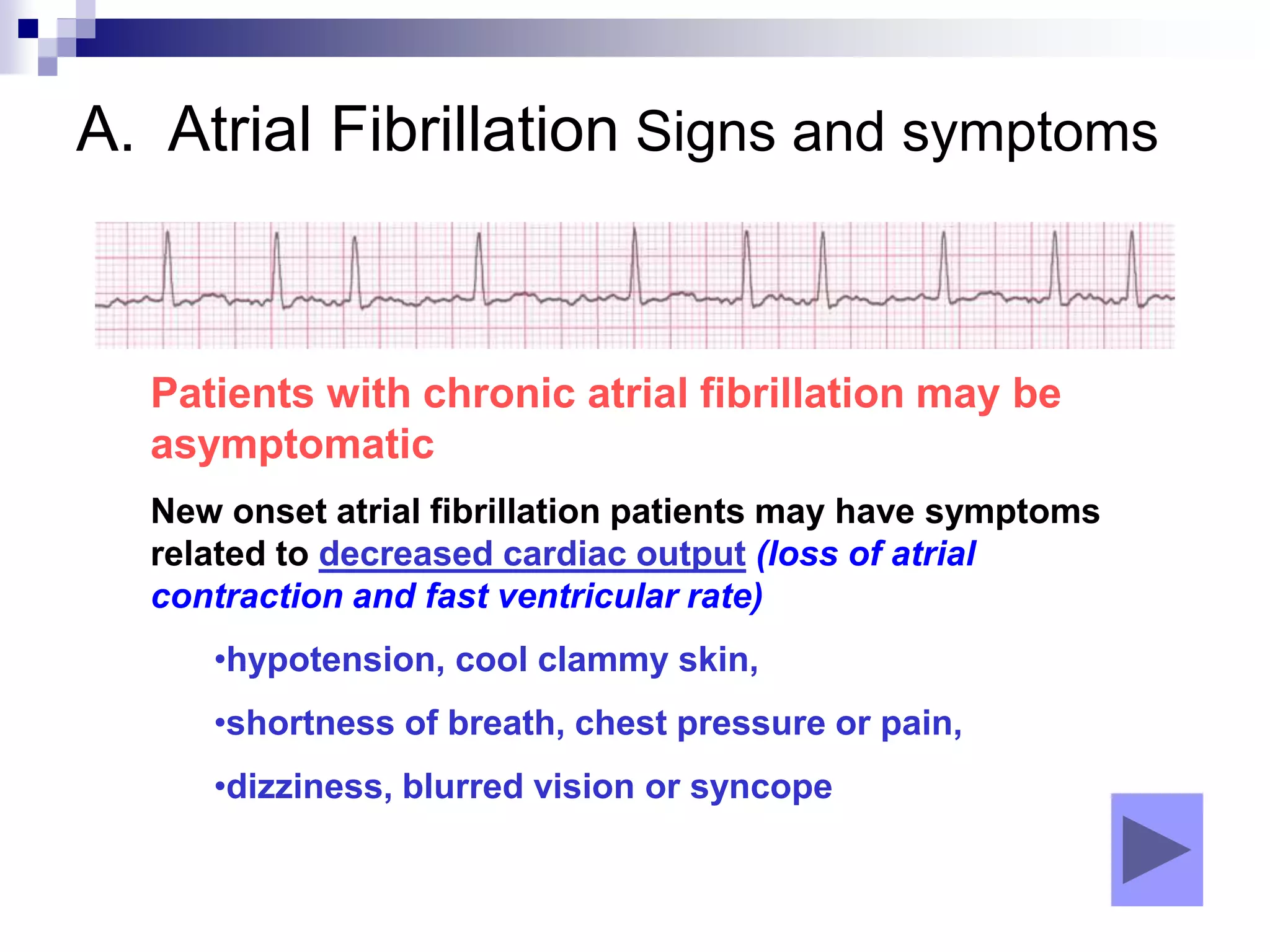
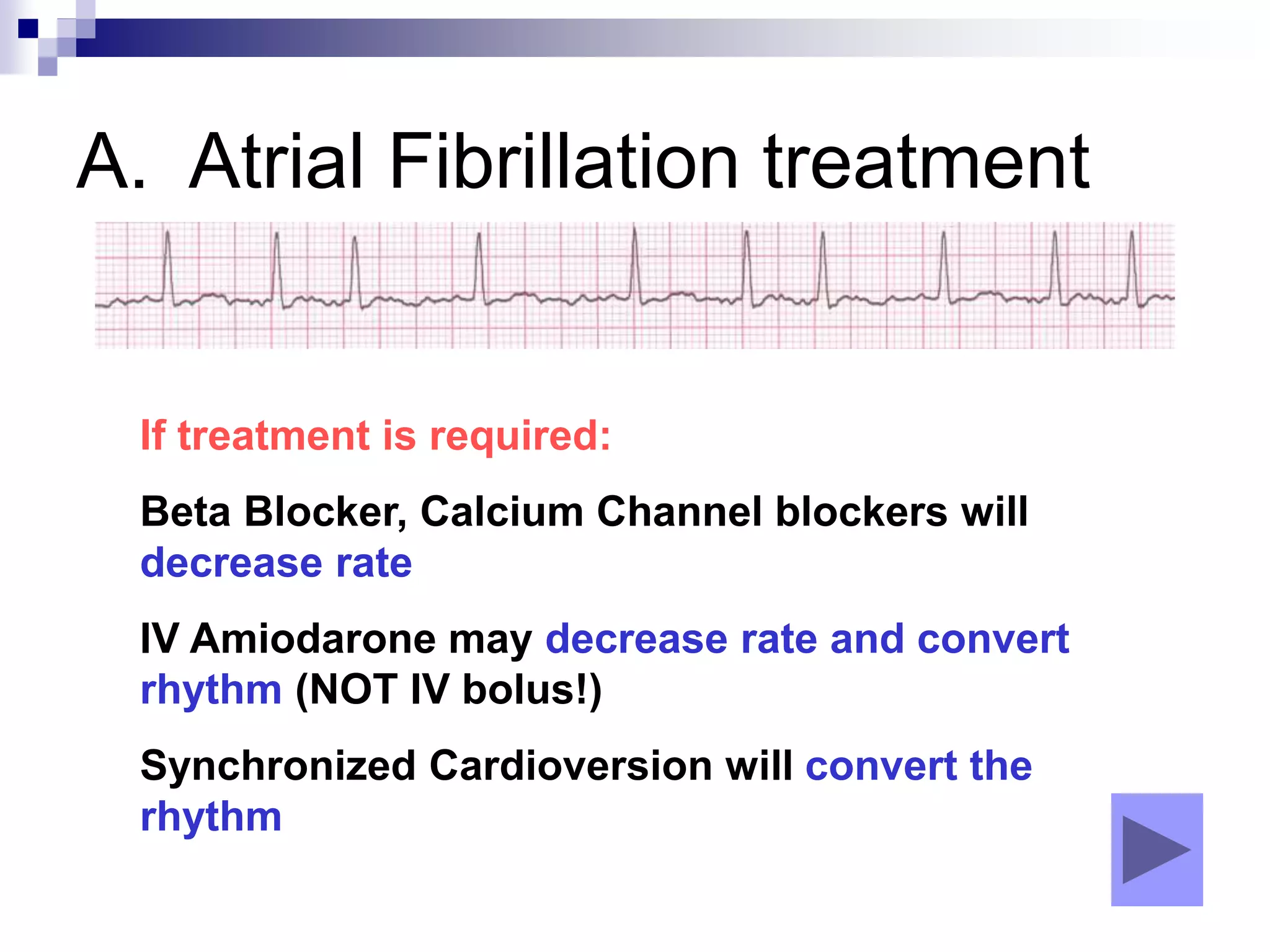
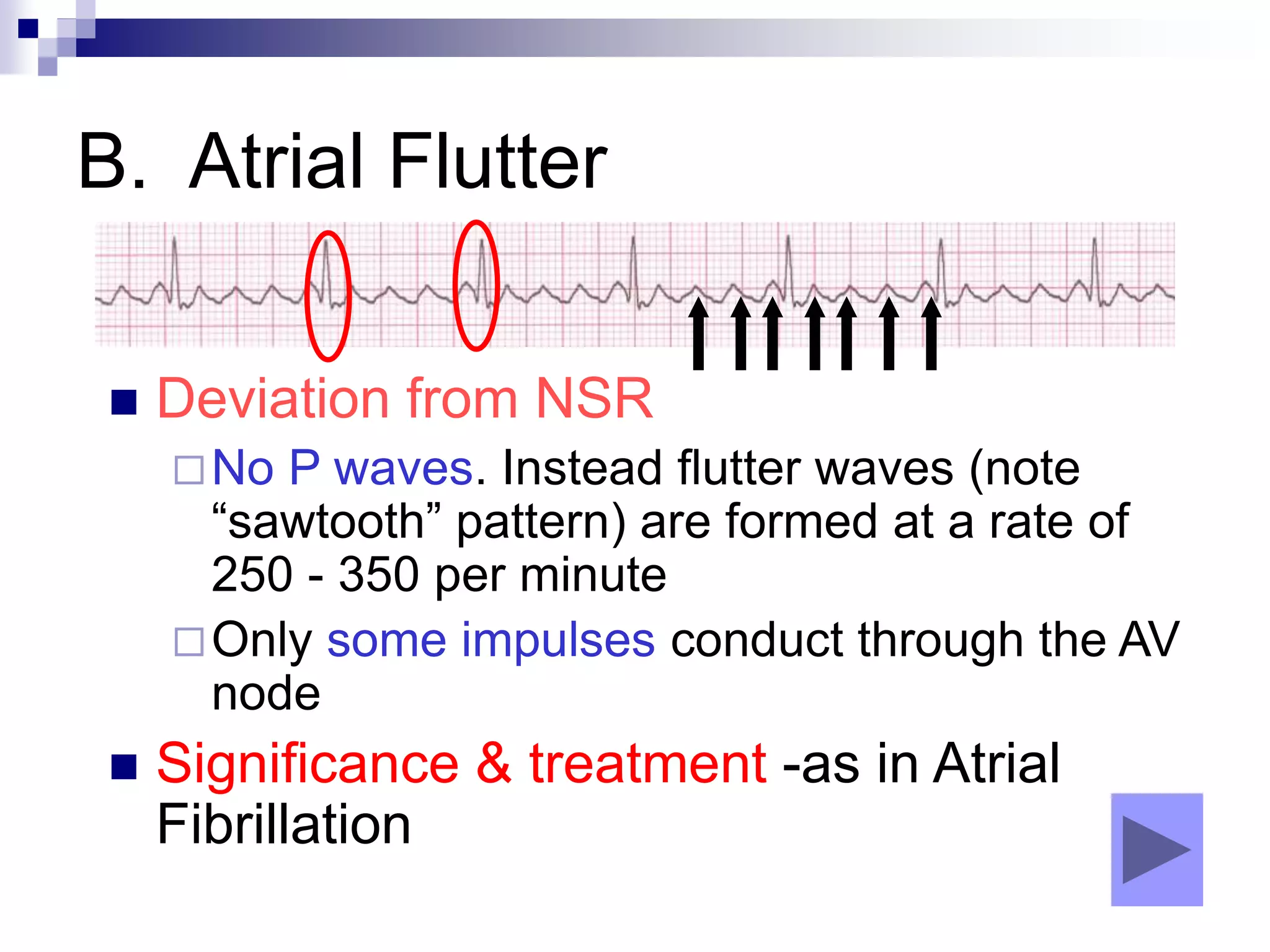
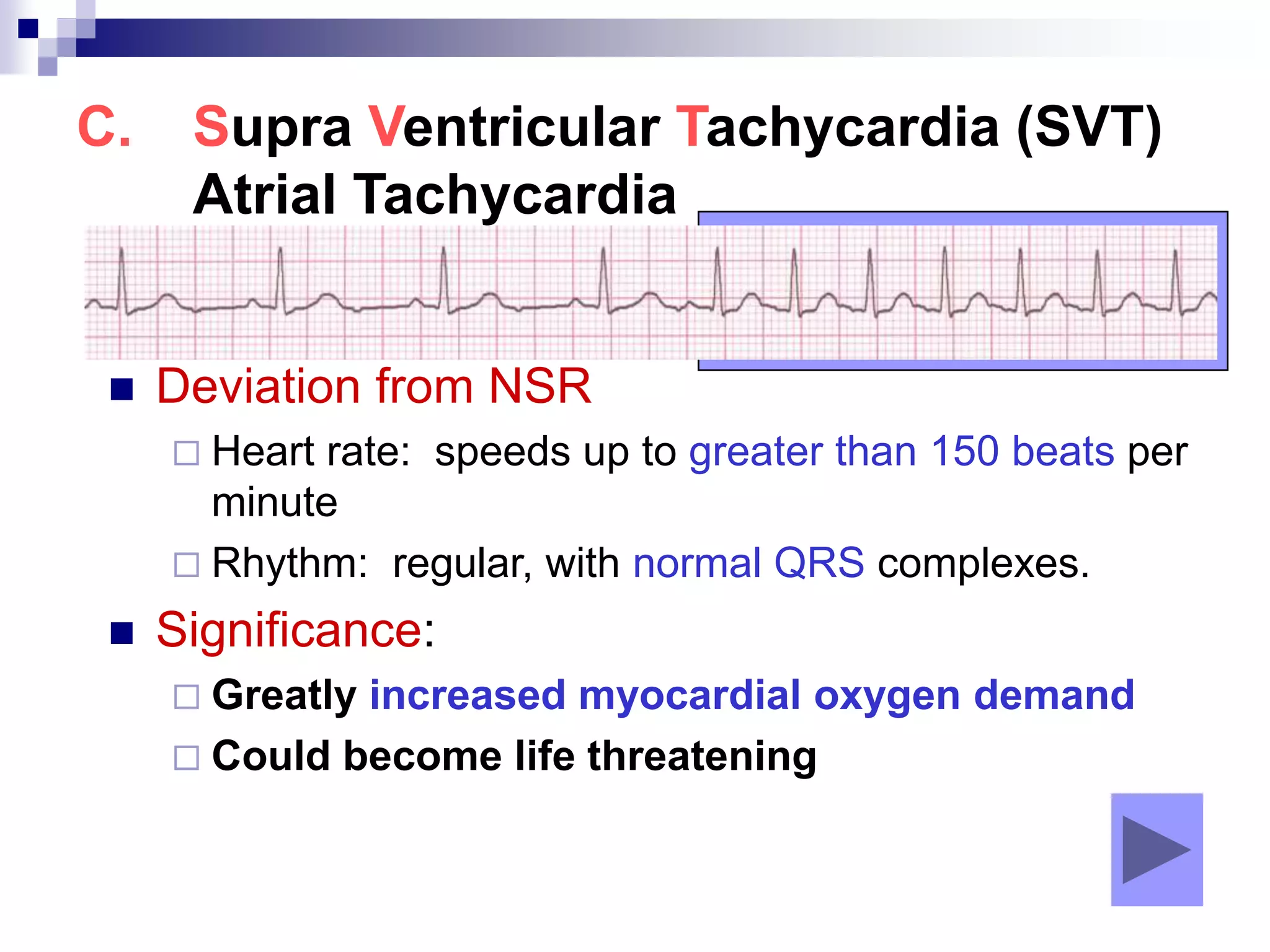
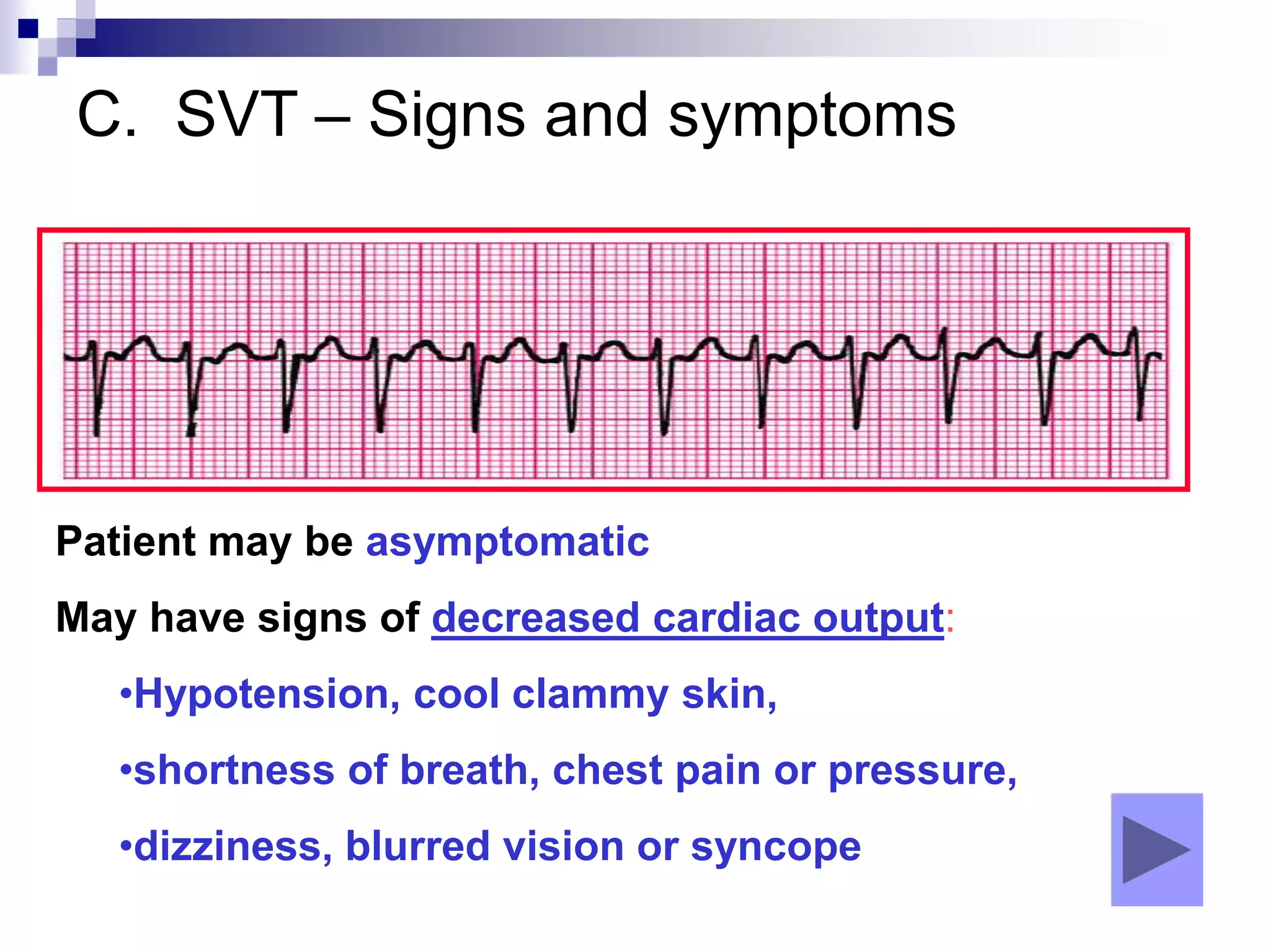
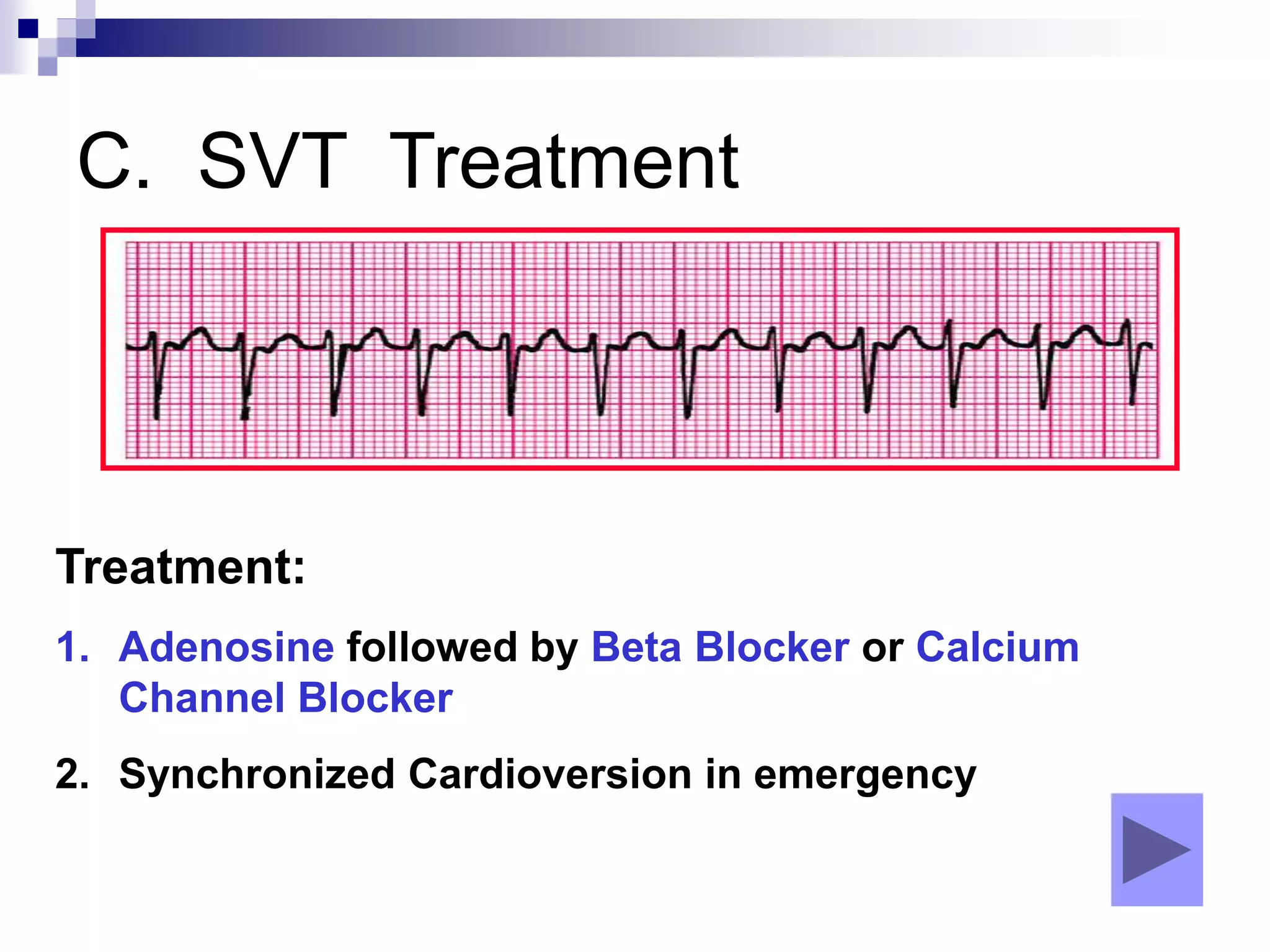
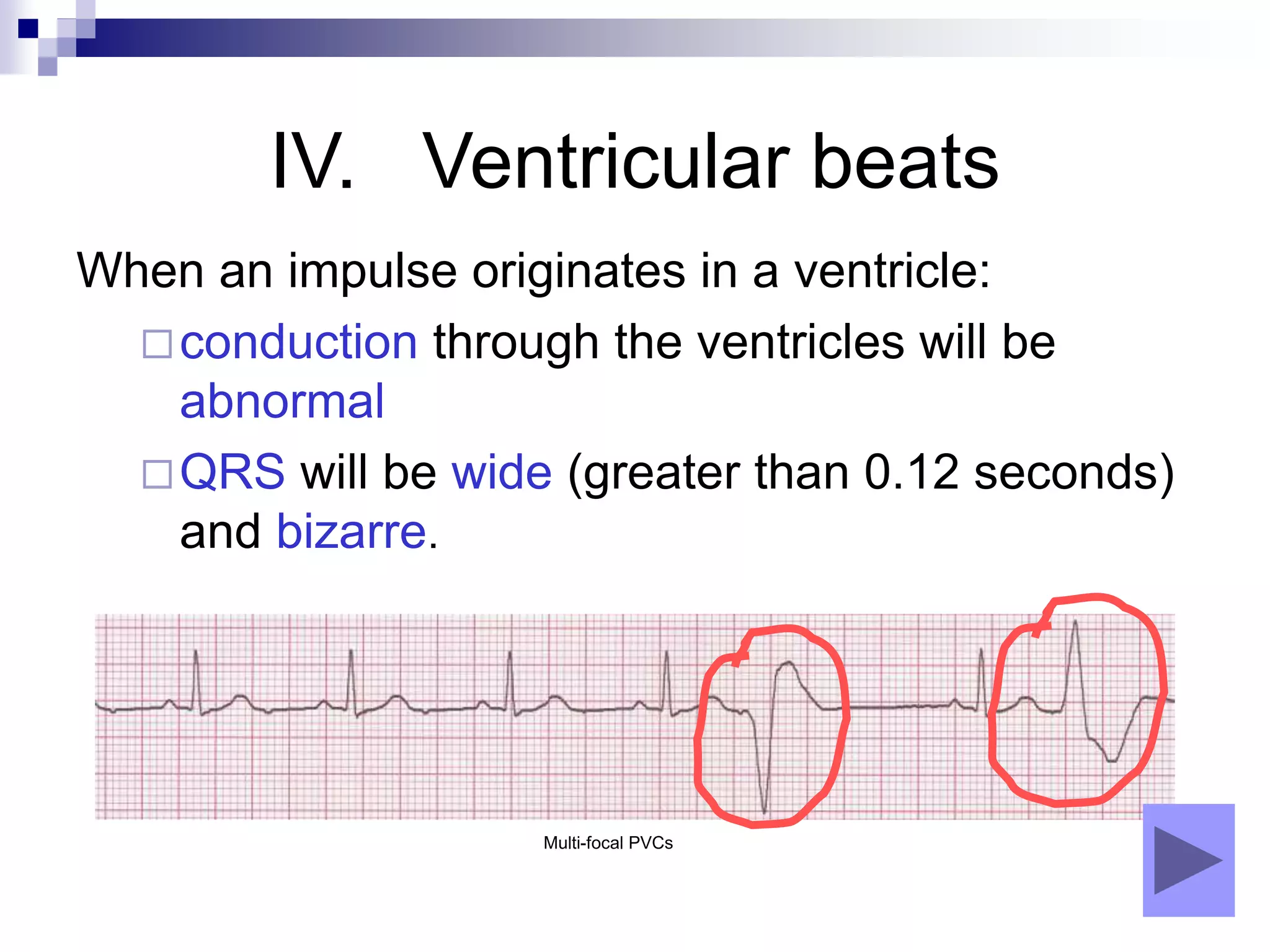
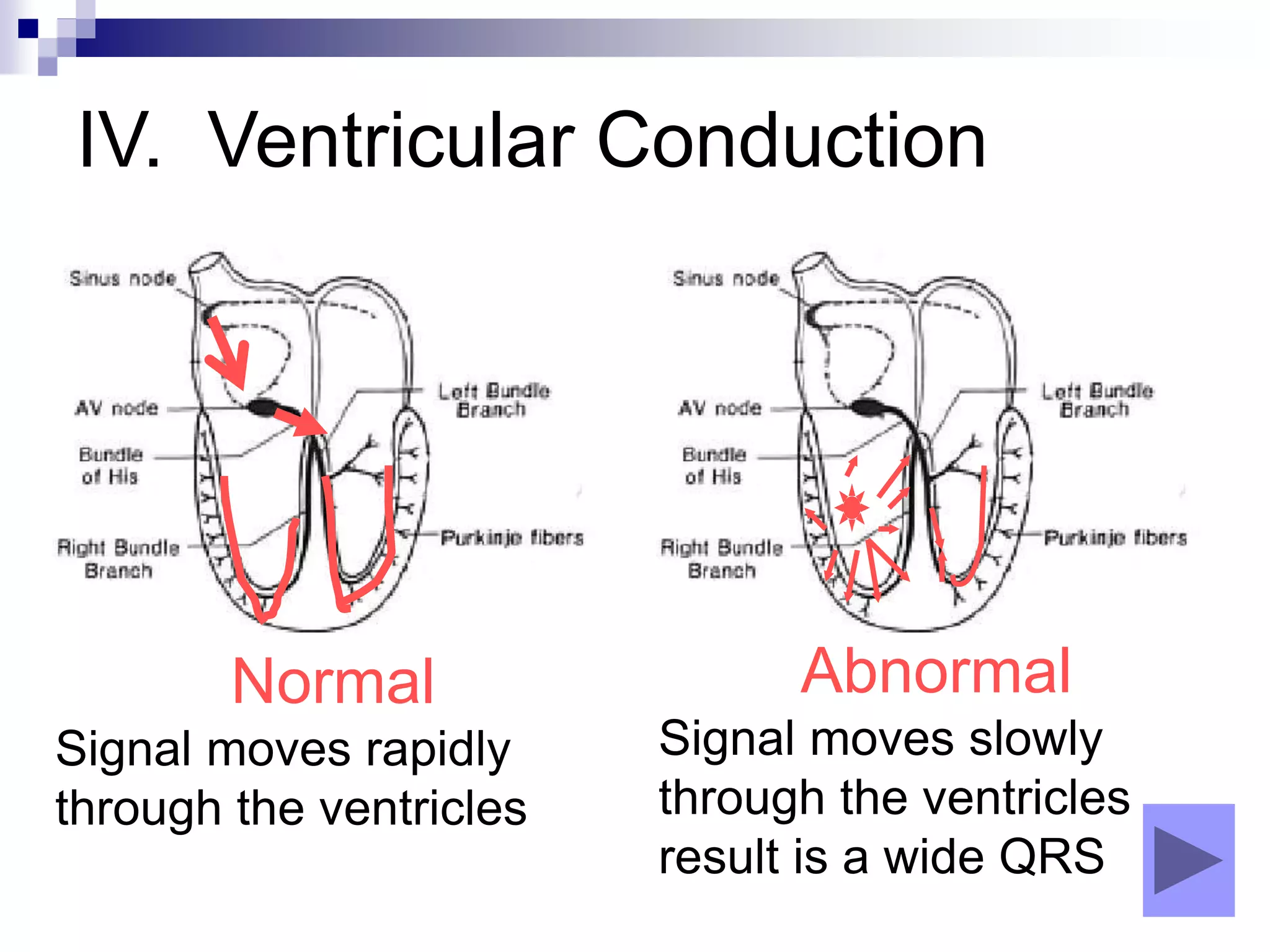
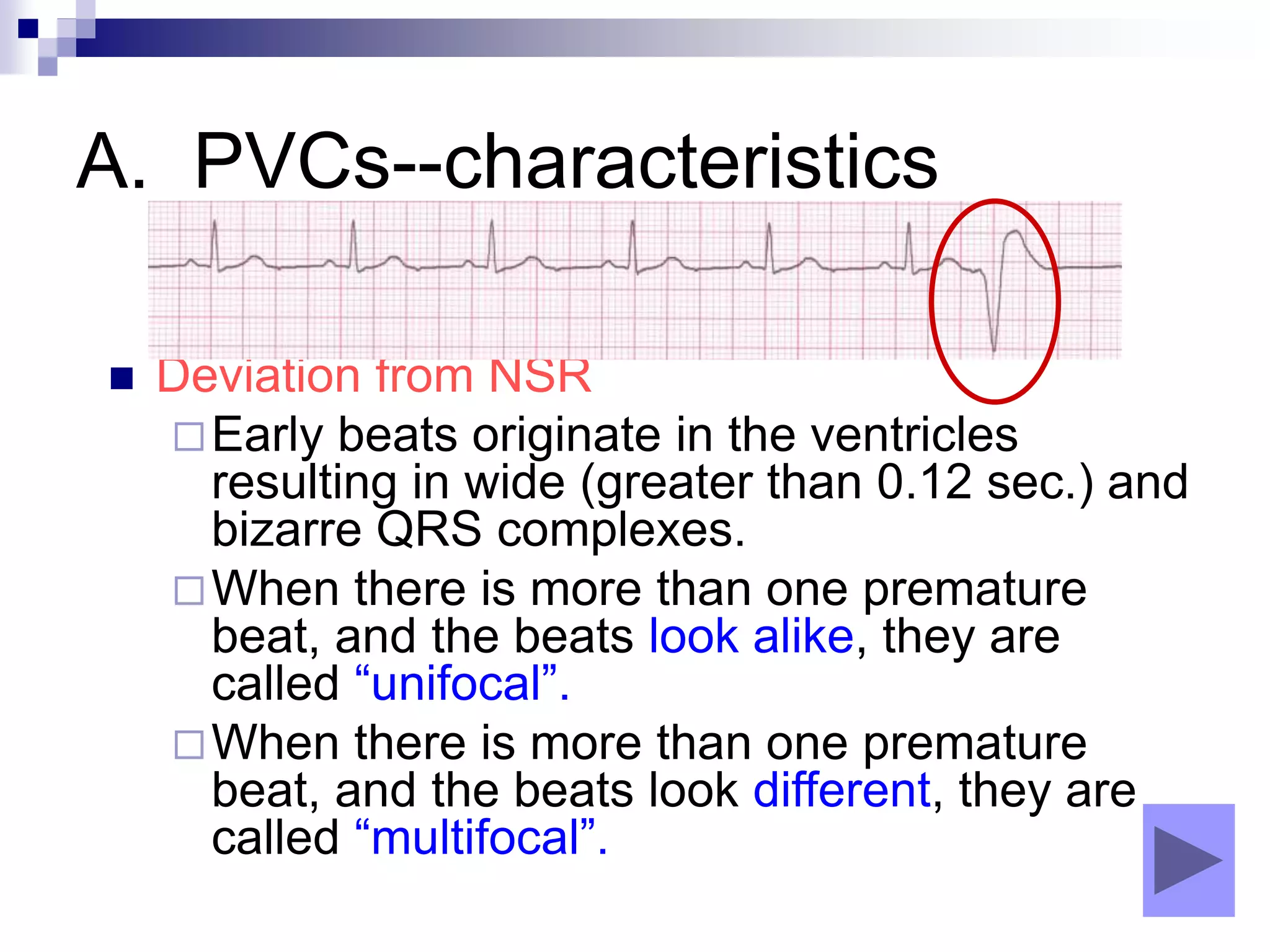
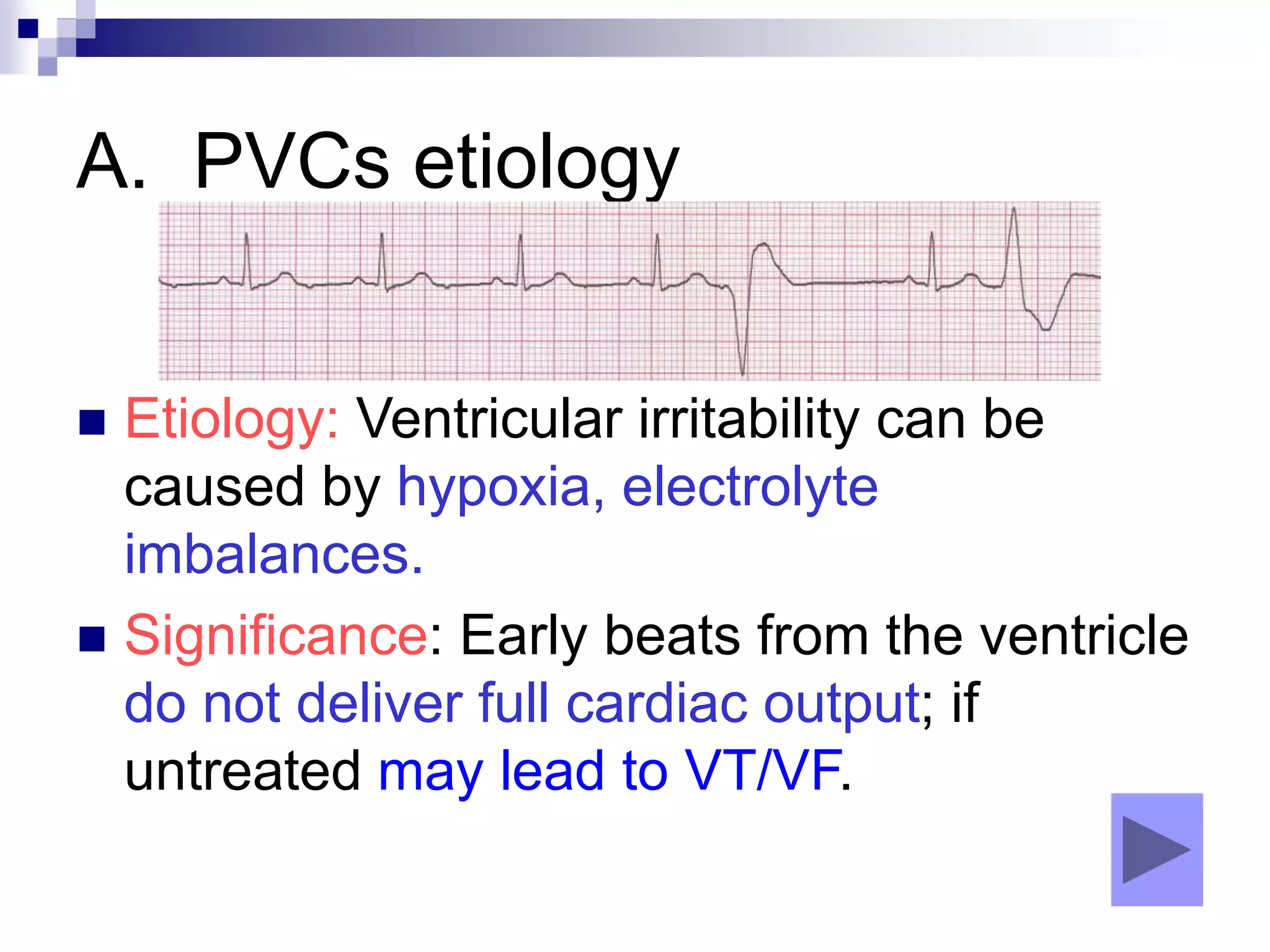
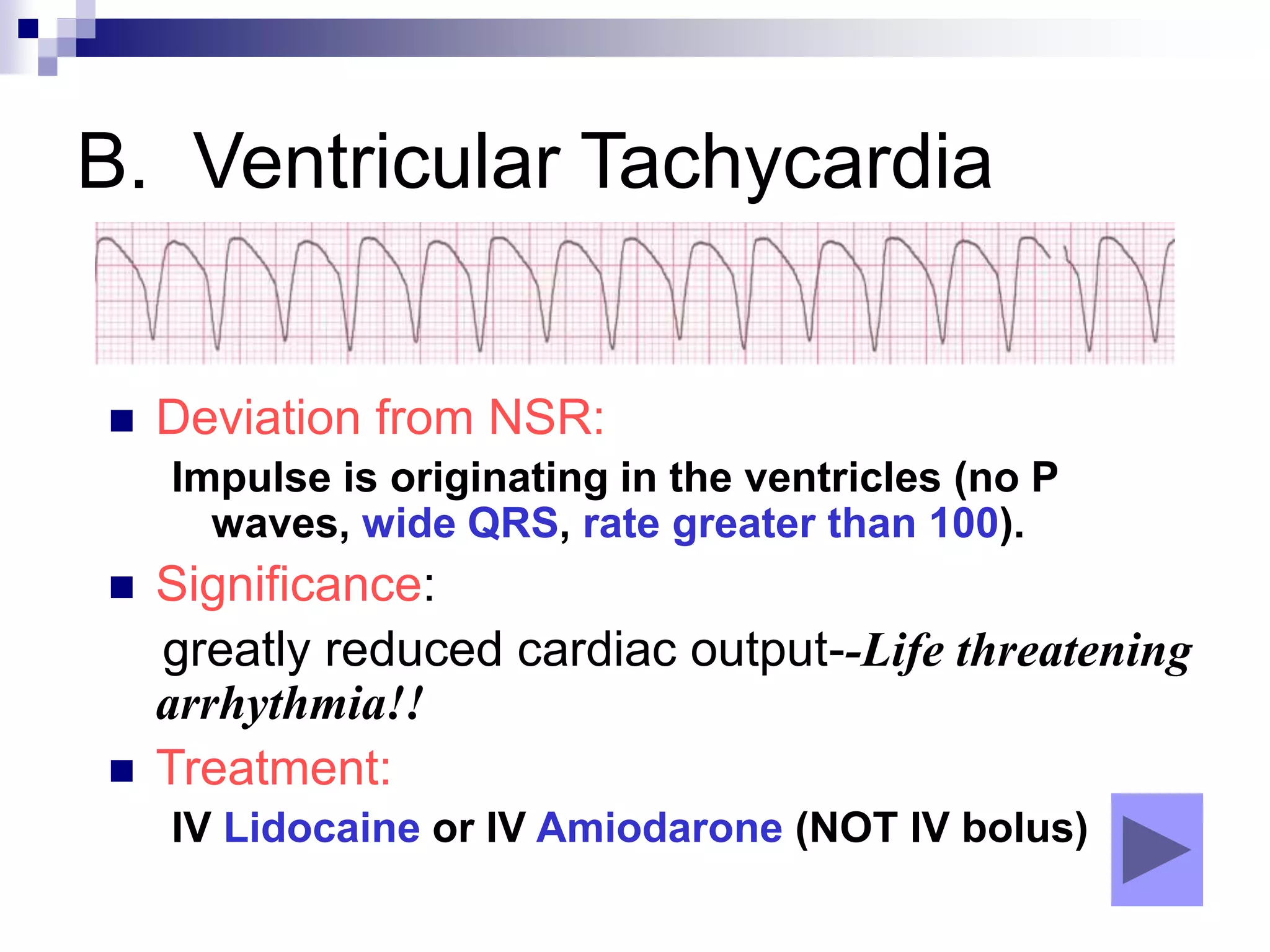
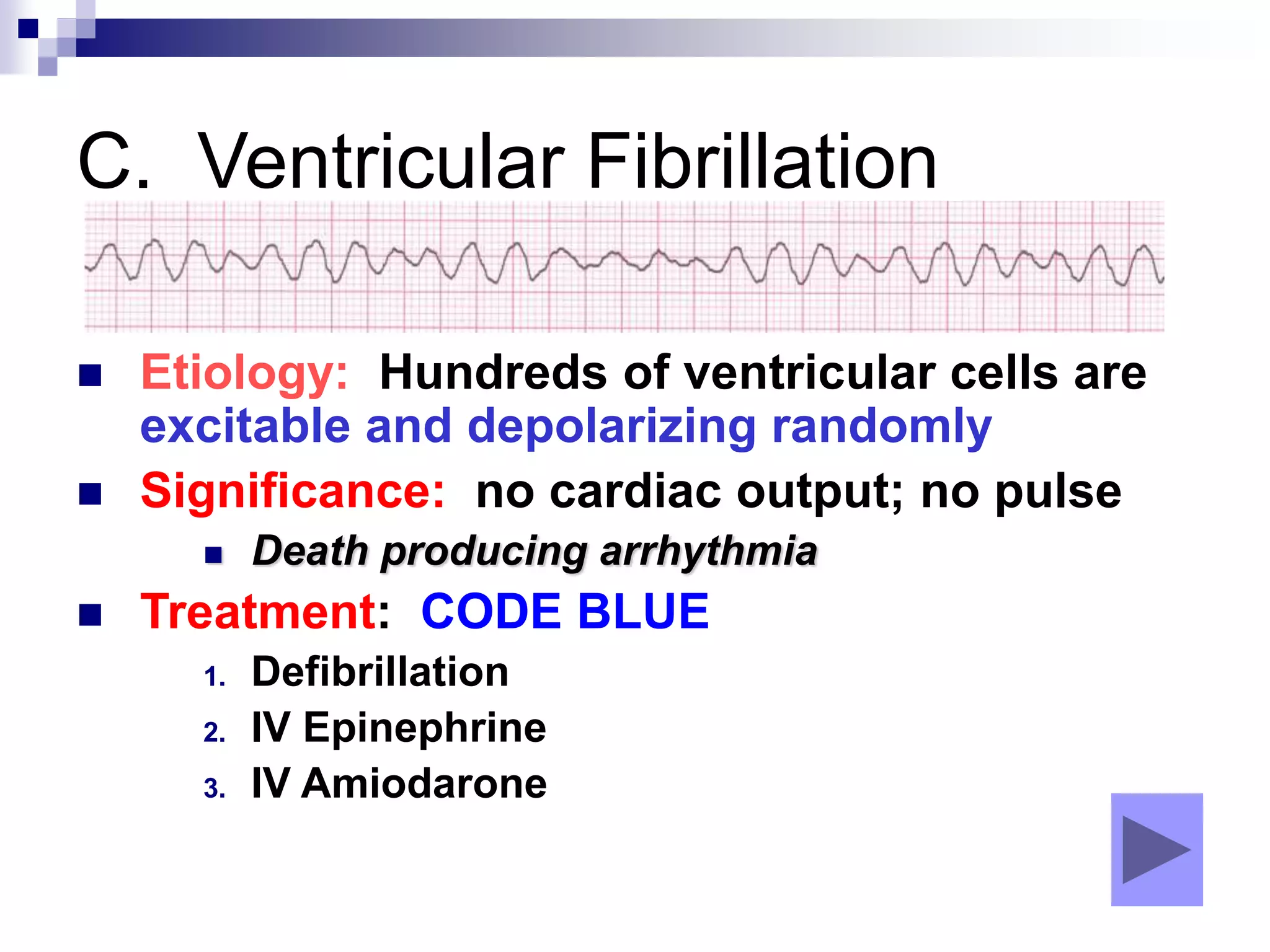
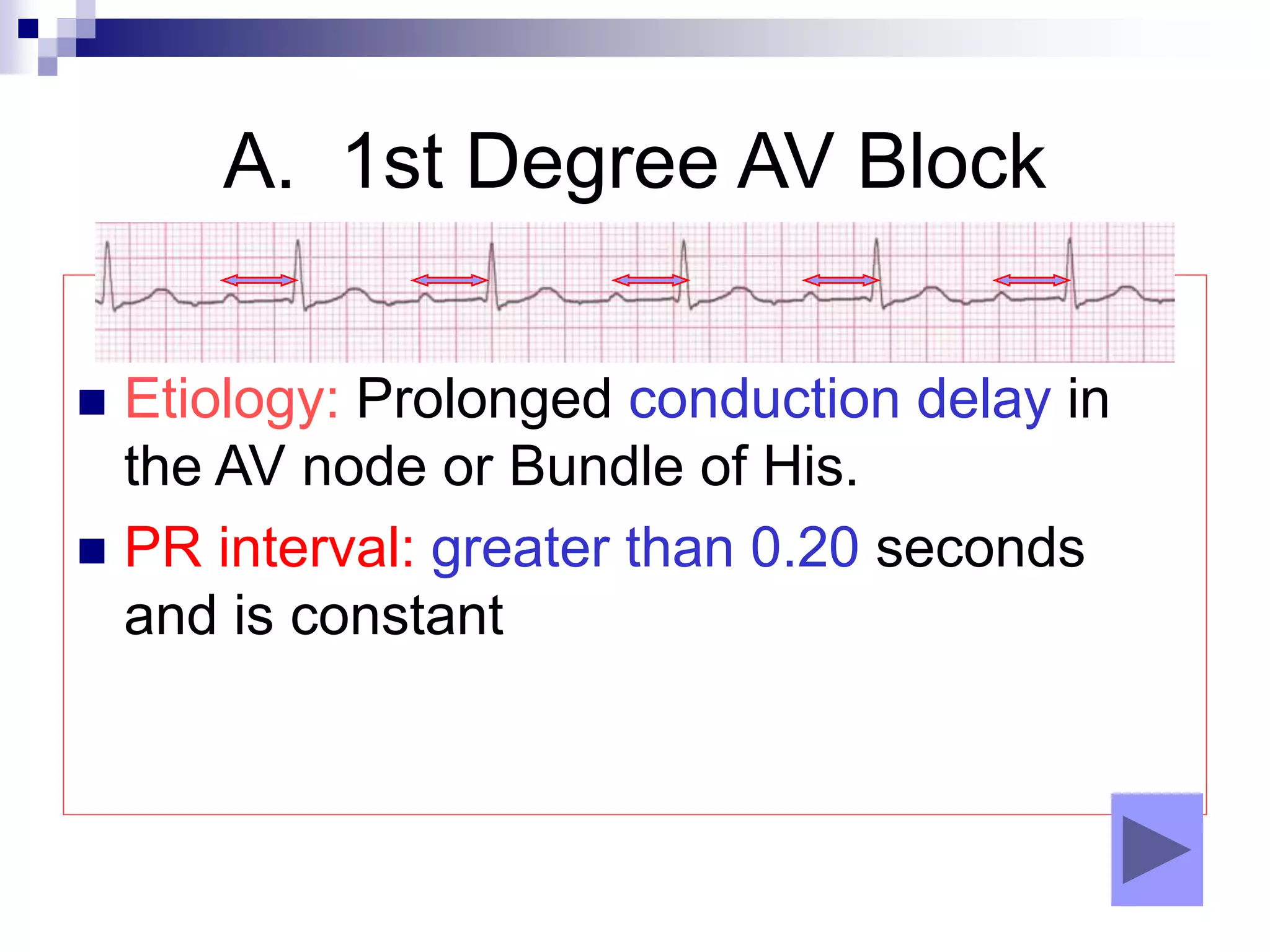
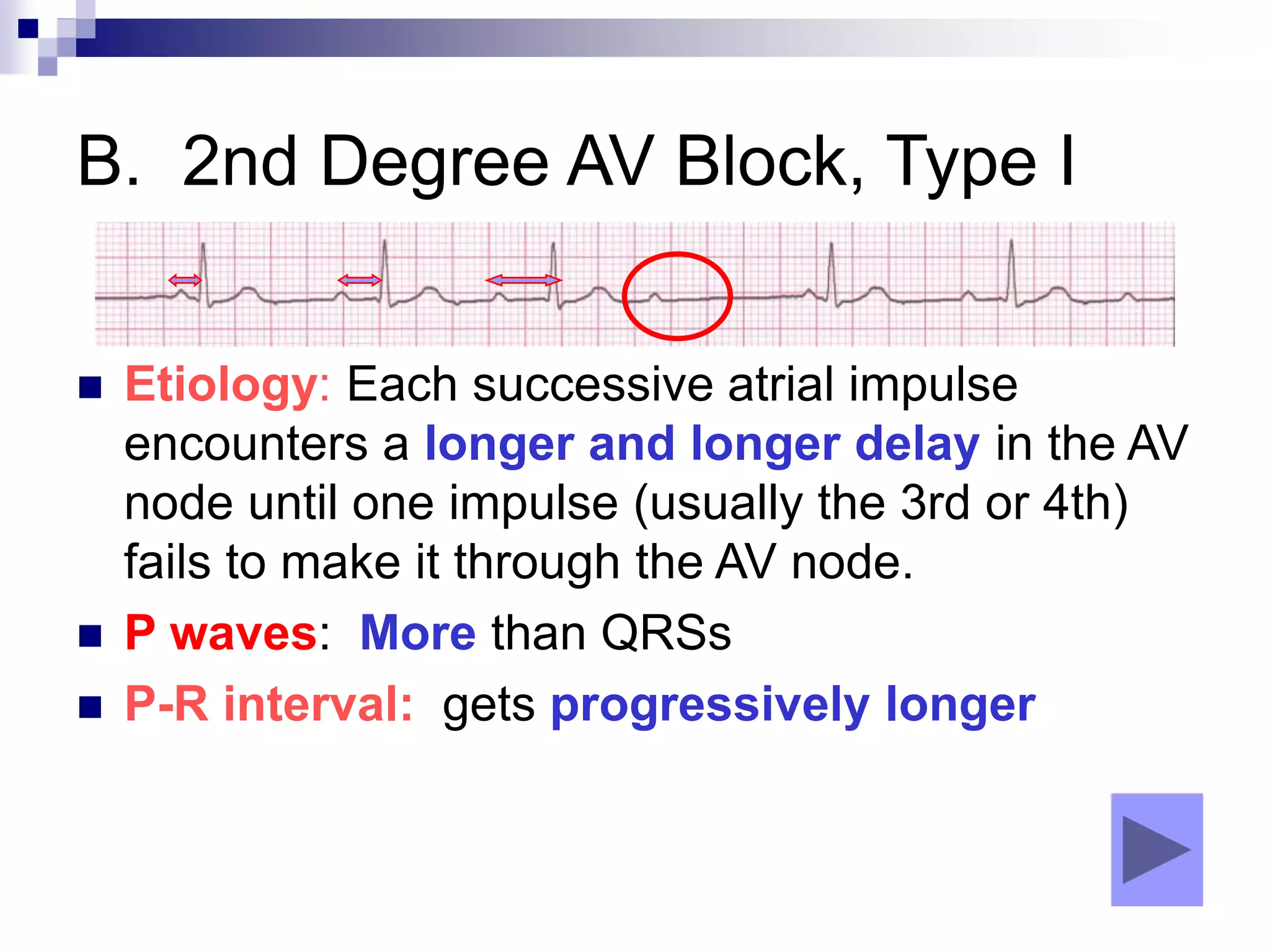
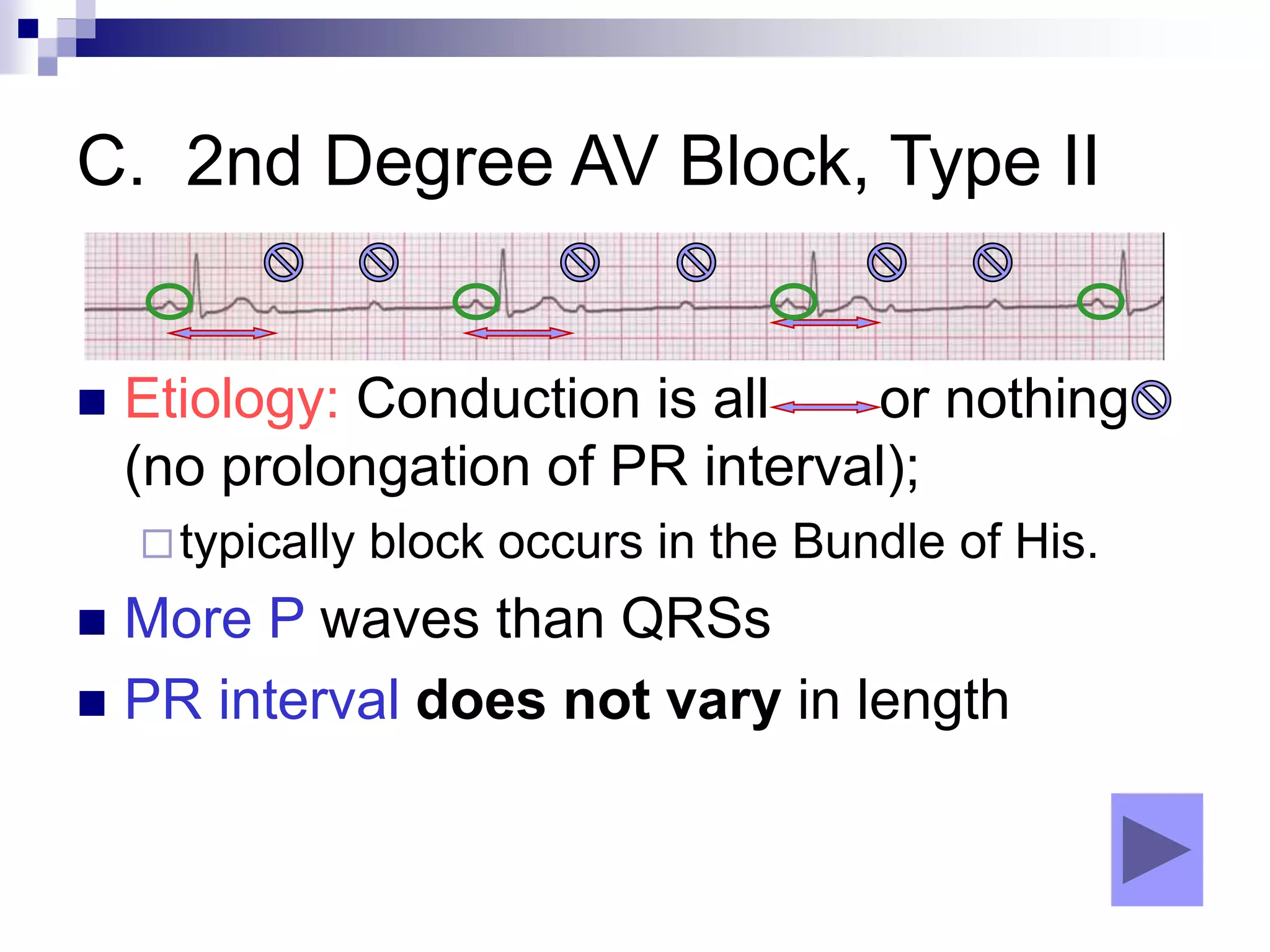
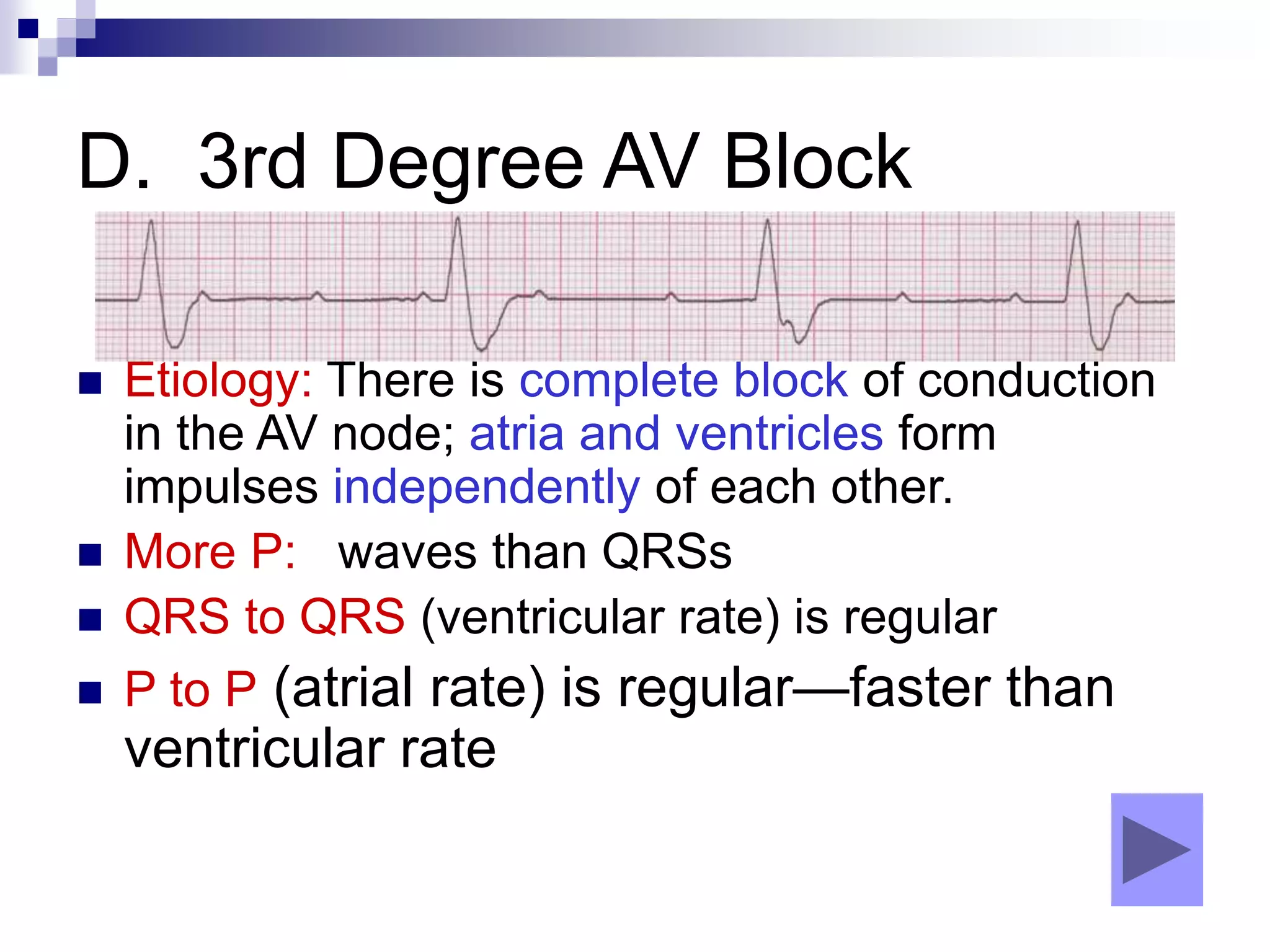
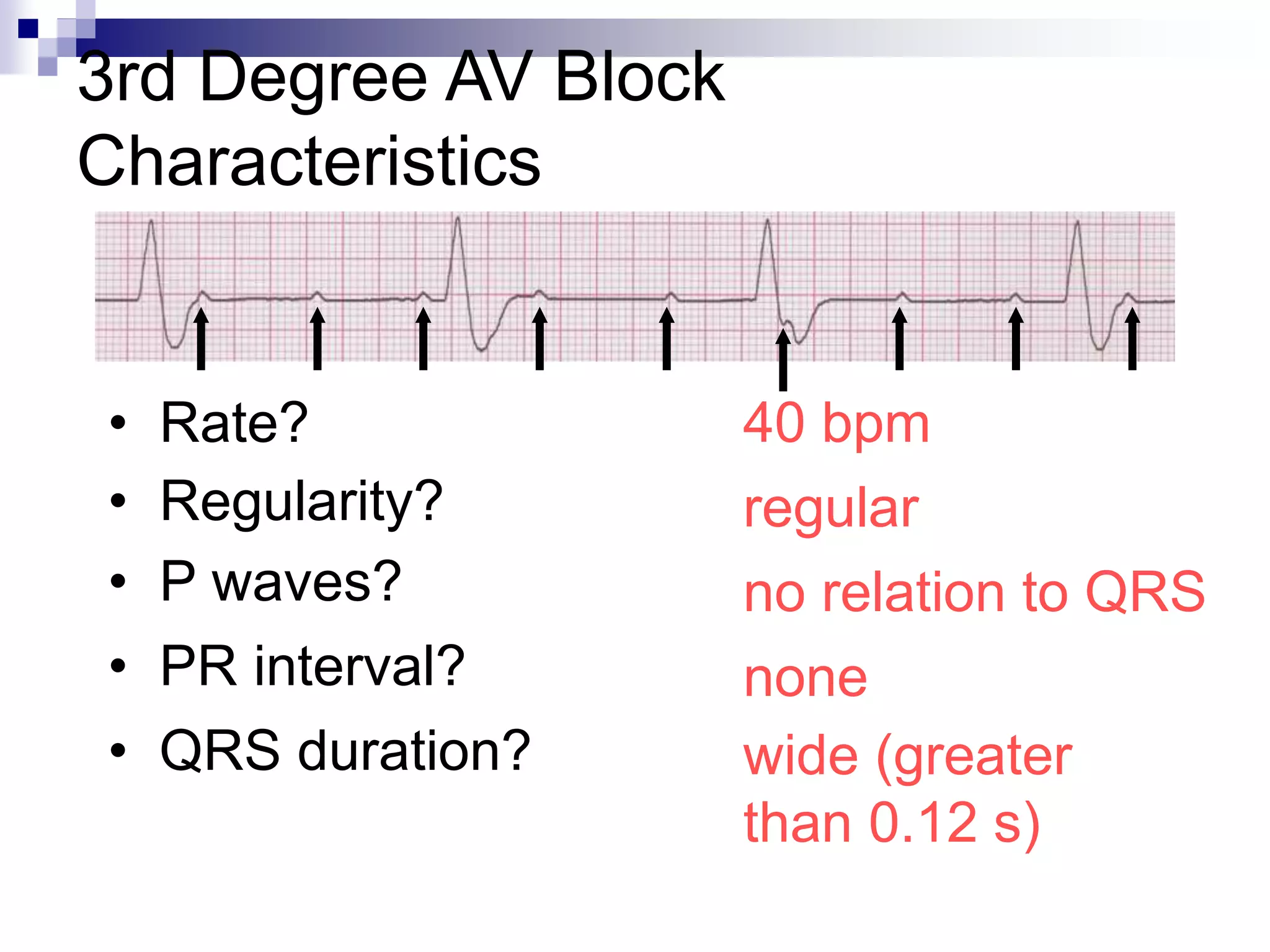
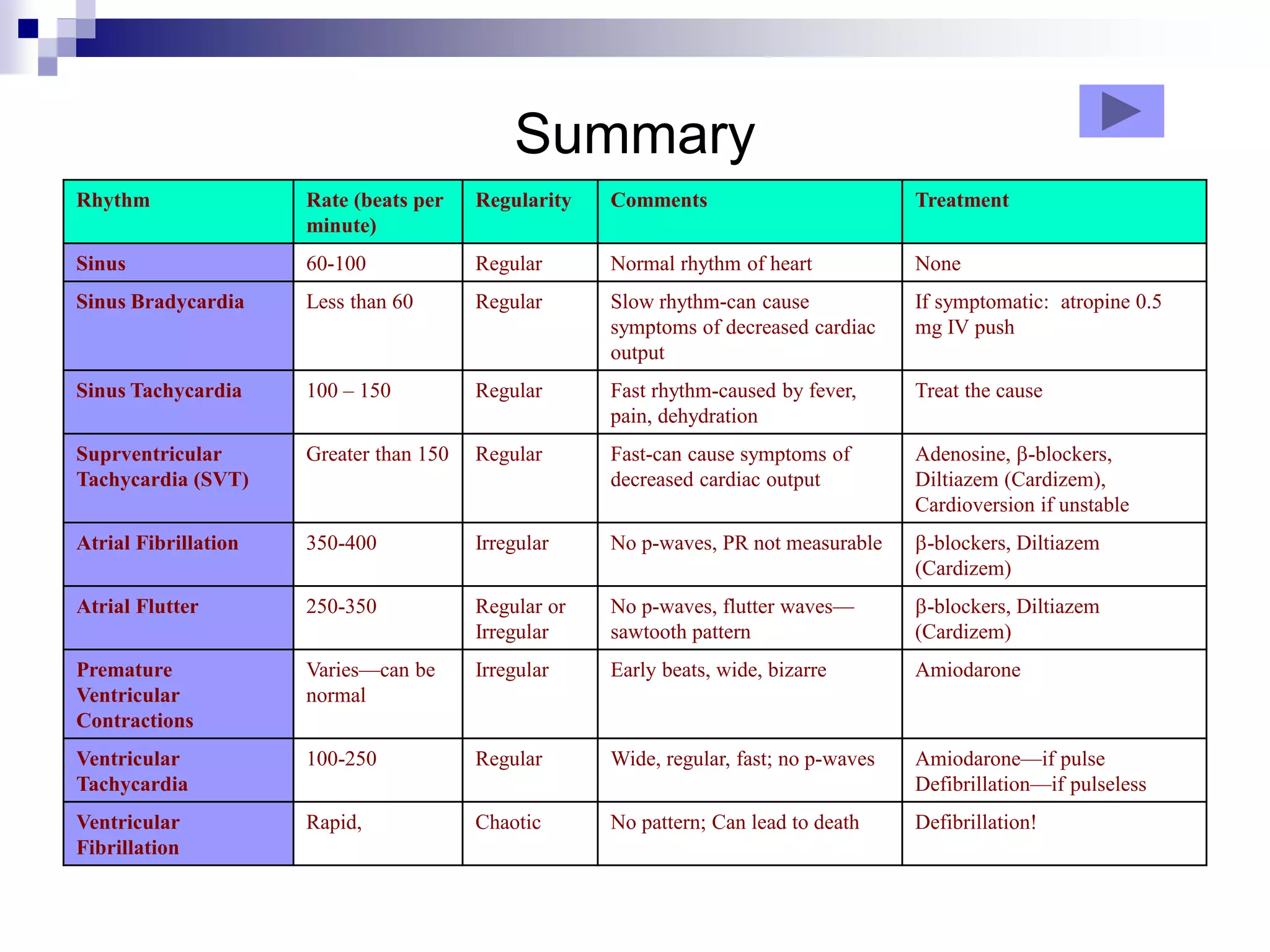
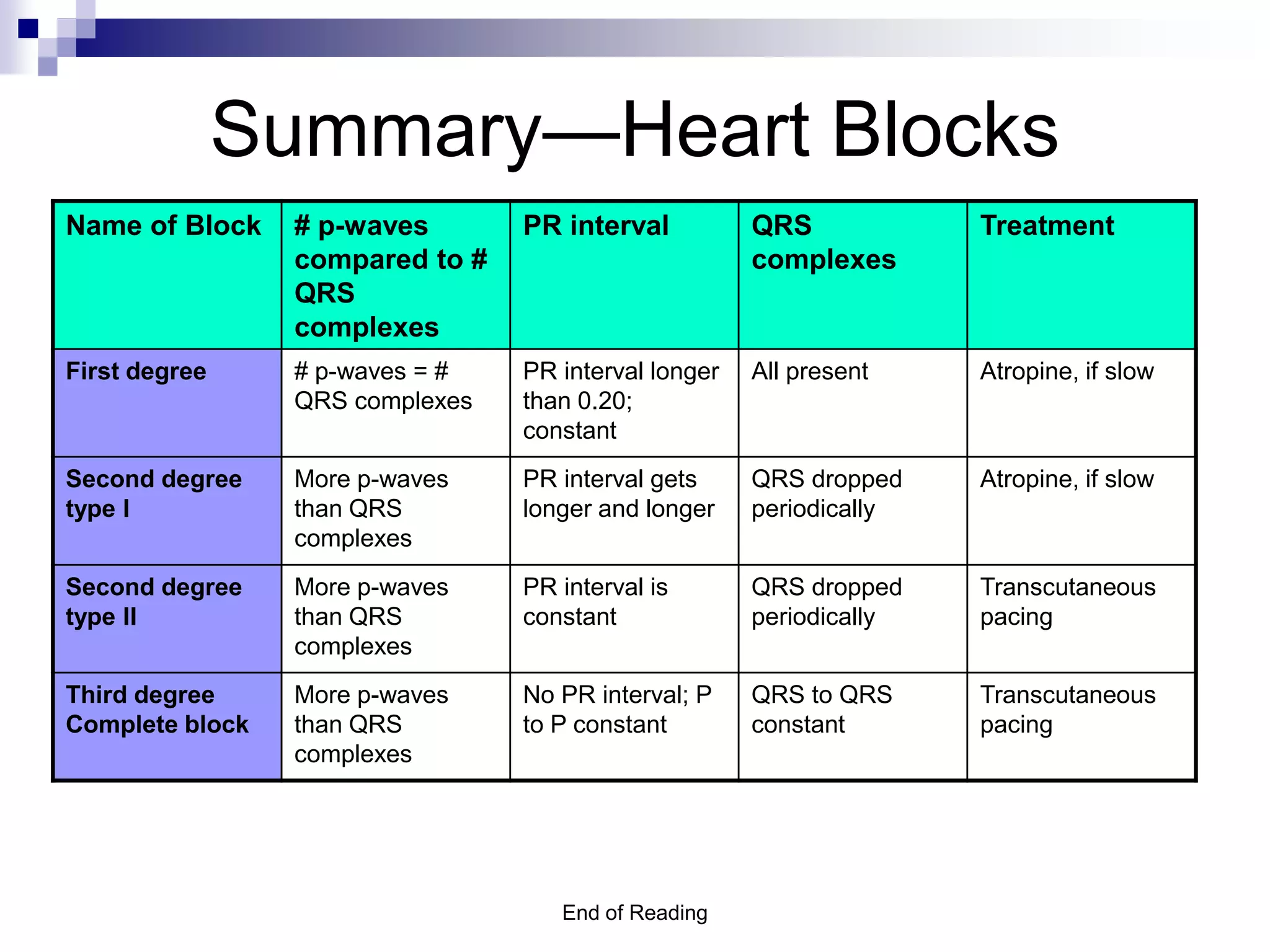
This document provides an overview of ECG rhythm interpretation. It discusses normal sinus rhythm and various arrhythmias including bradycardias related to problems with the sinus node or heart blocks. Tachycardias covered include sinus tachycardia, atrial fibrillation, atrial flutter, and supraventricular tachycardia. Premature ventricular contractions and ventricular tachycardia/fibrillation are also reviewed. For each rhythm abnormality, the document describes etiology, characteristics, signs/symptoms and treatment approaches.