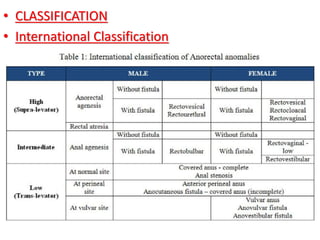
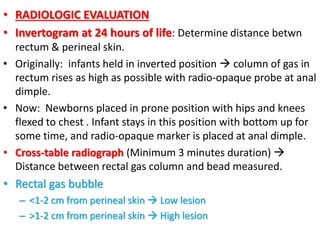
This document discusses anorectal malformations (ARMs), which occur in approximately 1 in 4,000 to 5,000 births. ARMs can be low or high lesions depending on whether the rectum has descended through the sphincter complex. Surgical techniques for repair include primary repair for perineal/vestibular fistulas or staged repair for more complex cases involving diverting colostomy, definitive reconstruction, and later colostomy closure. Outcomes depend on the extent and nature of the anomaly as well as surgical expertise, with risks including urinary/fecal incontinence. Thorough evaluation and thoughtful surgical care are important to determine the future of children born with ARMs.