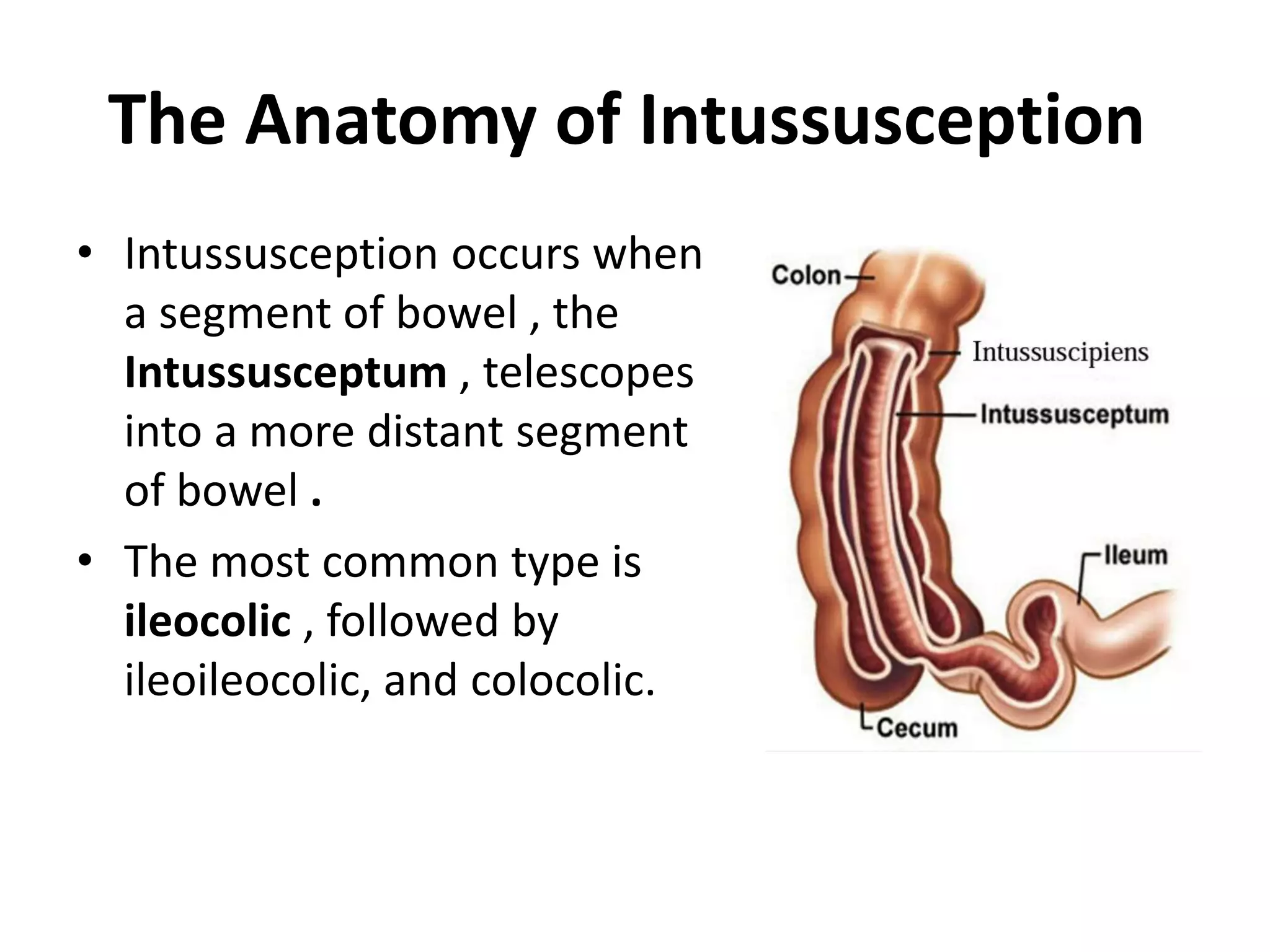
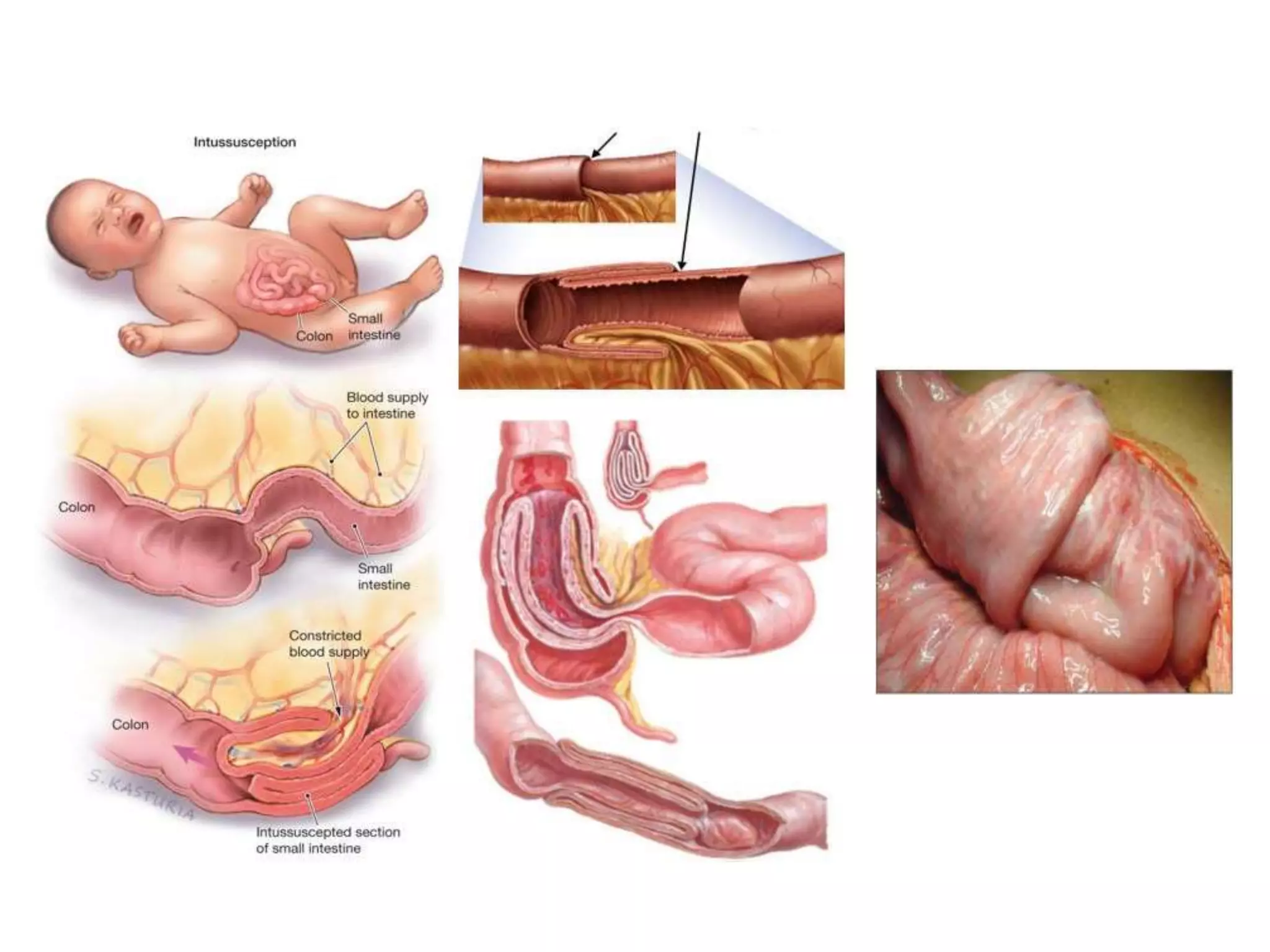
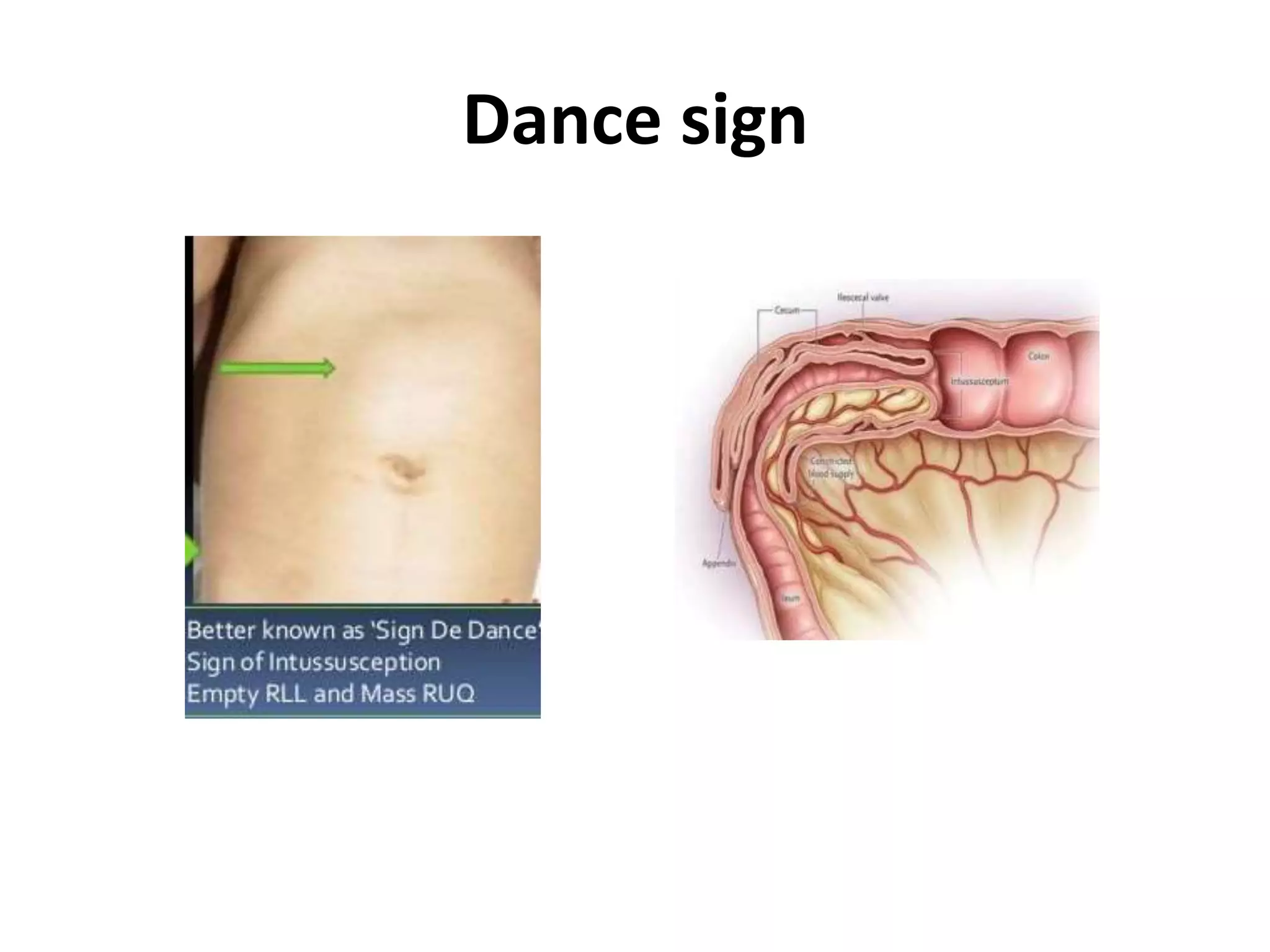
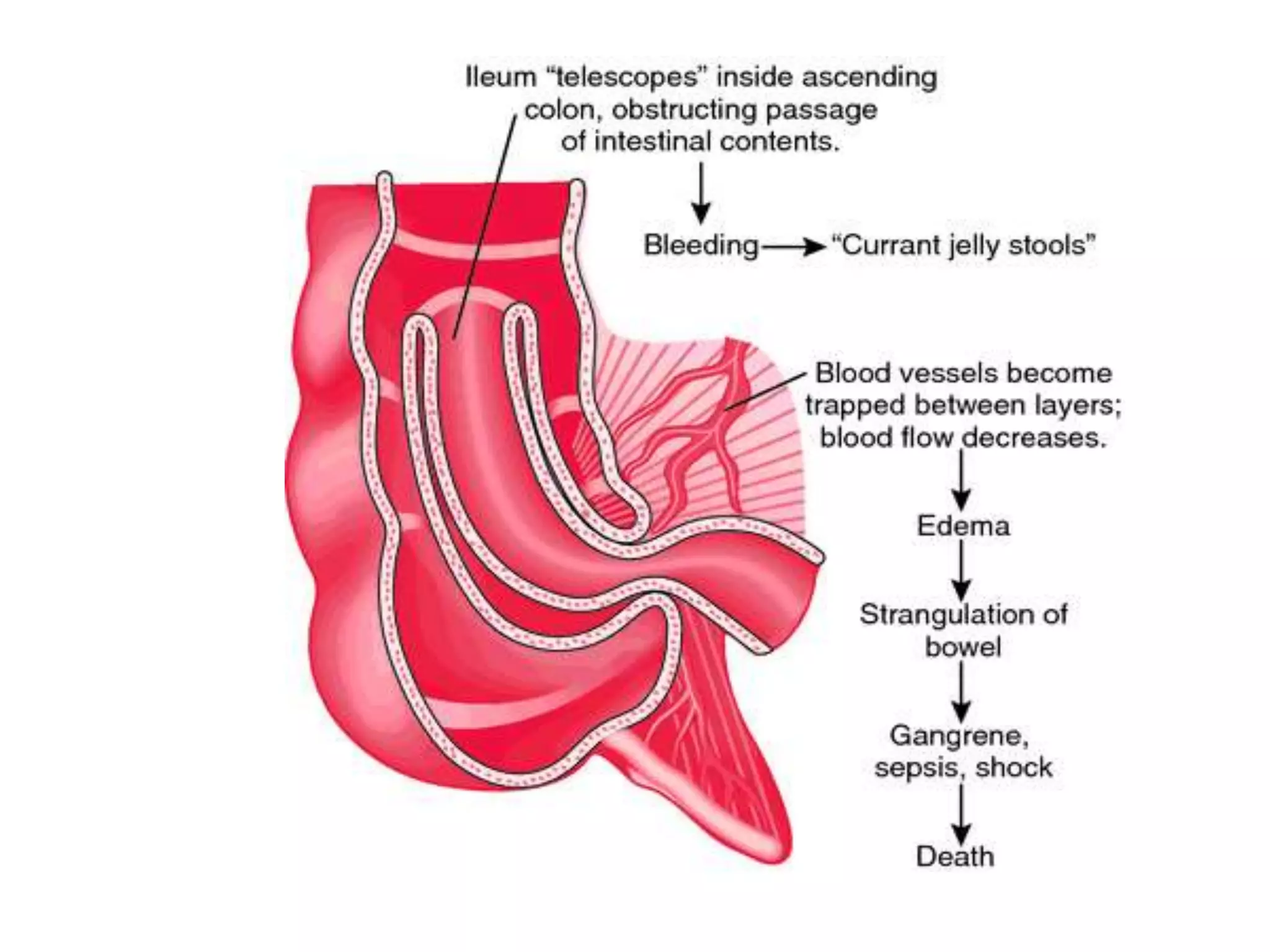
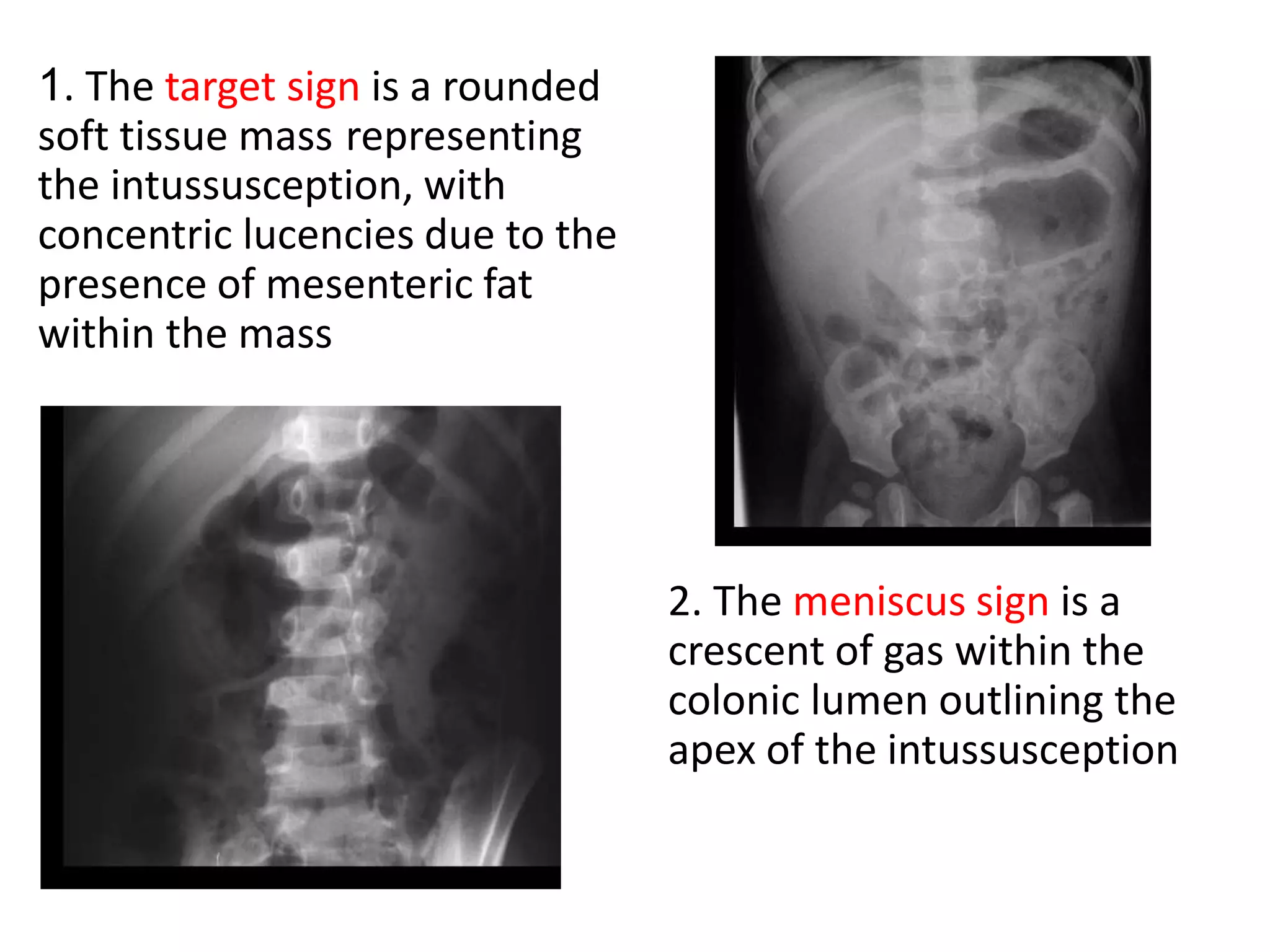
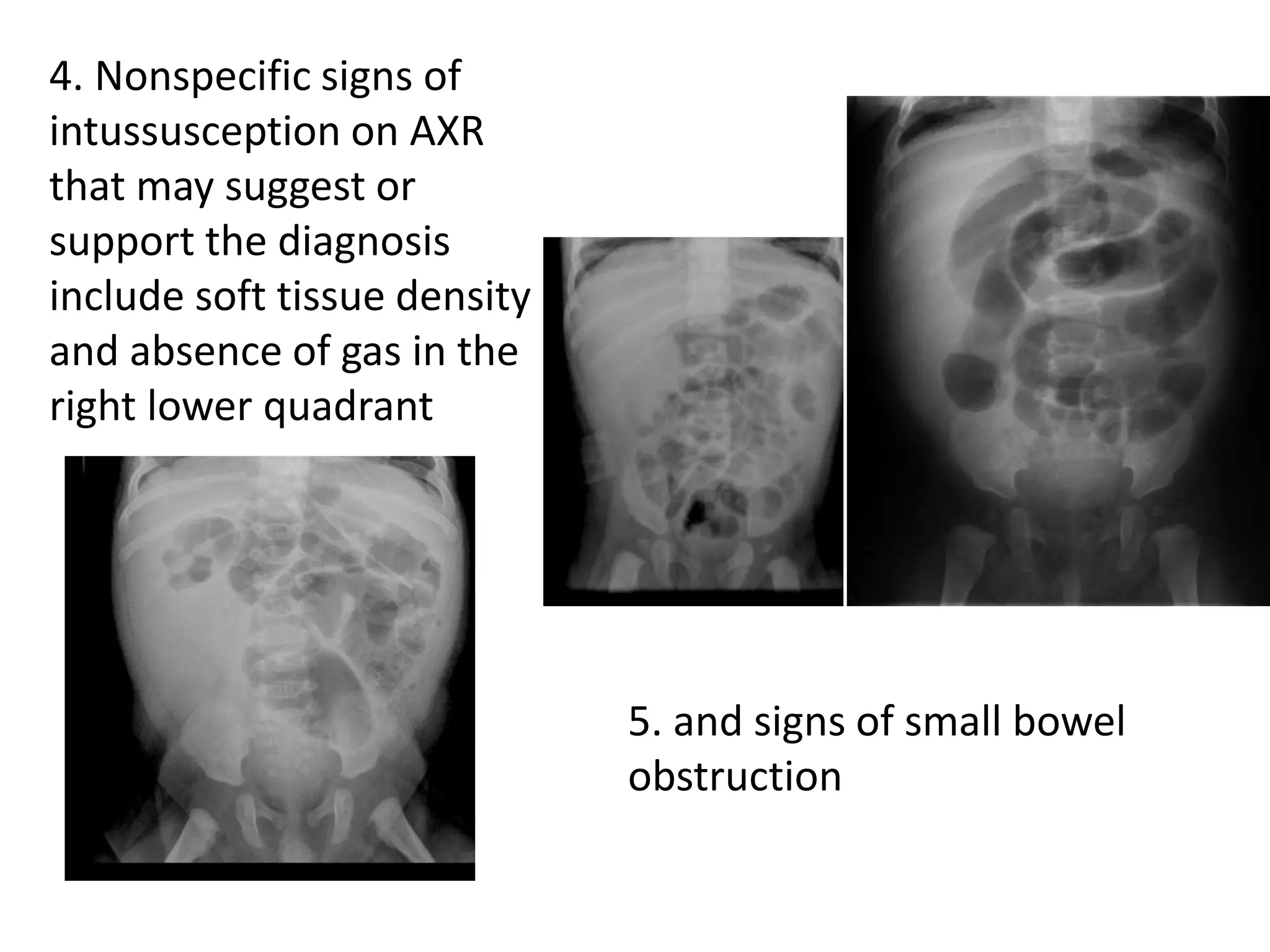
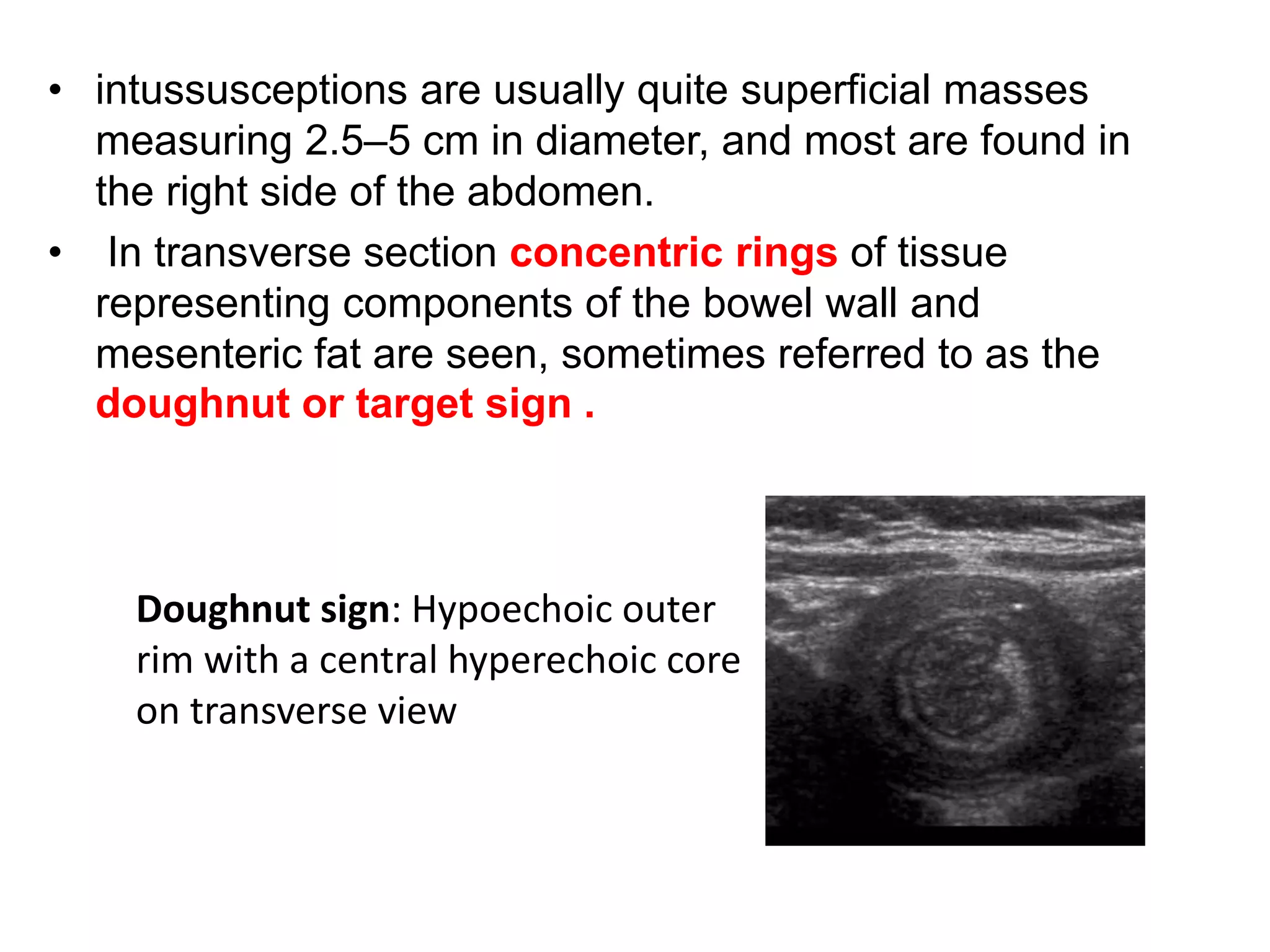
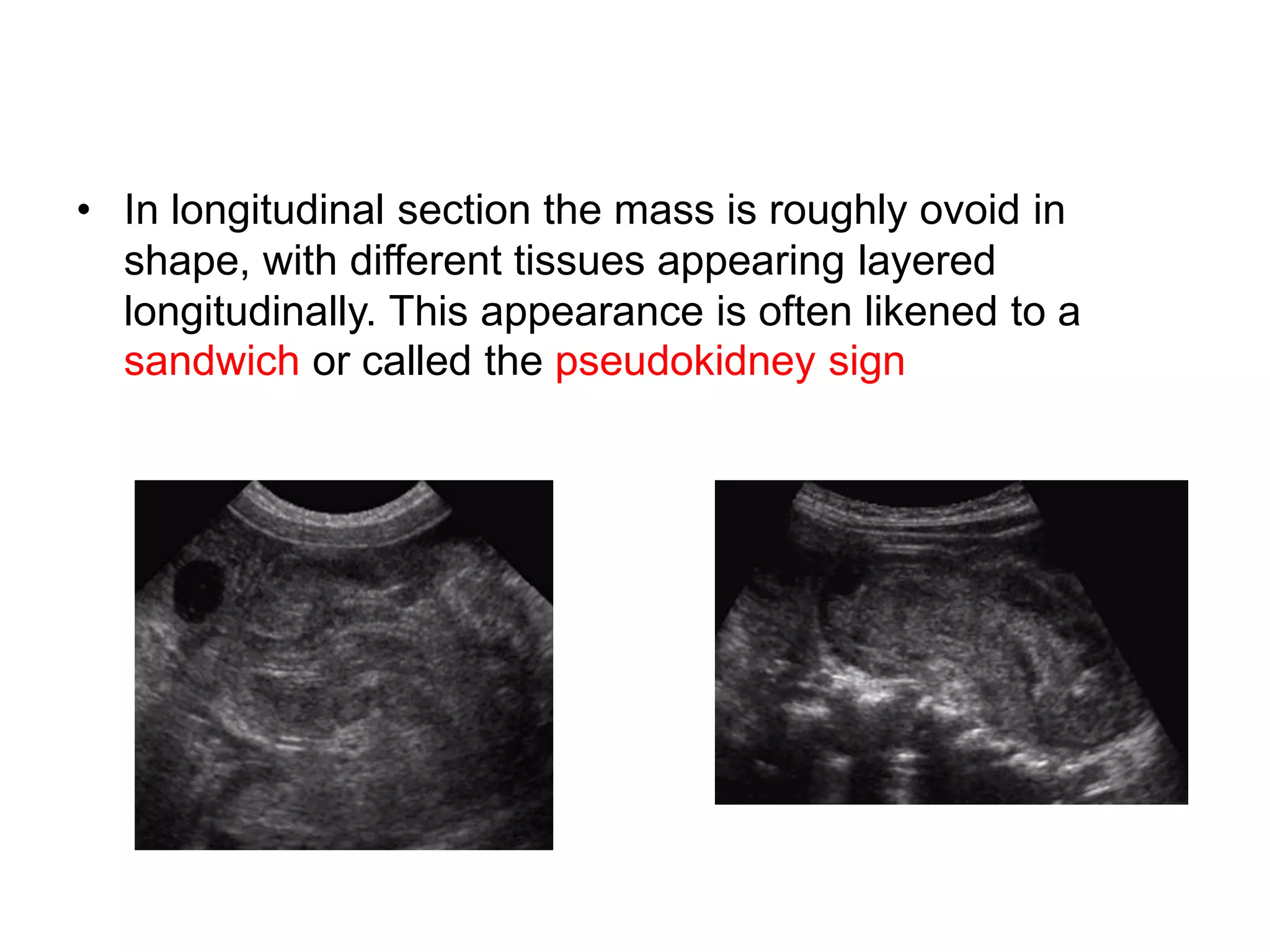
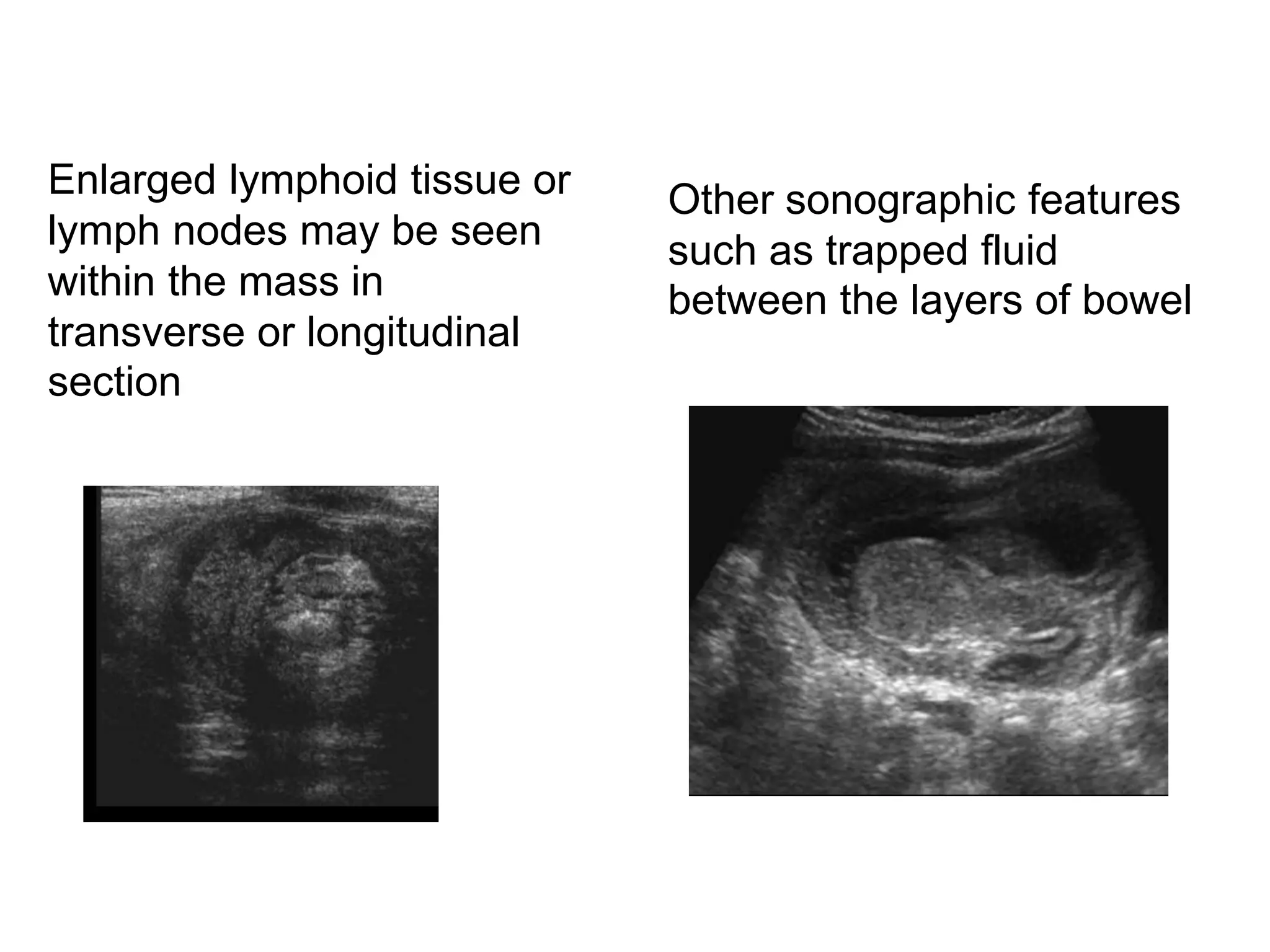
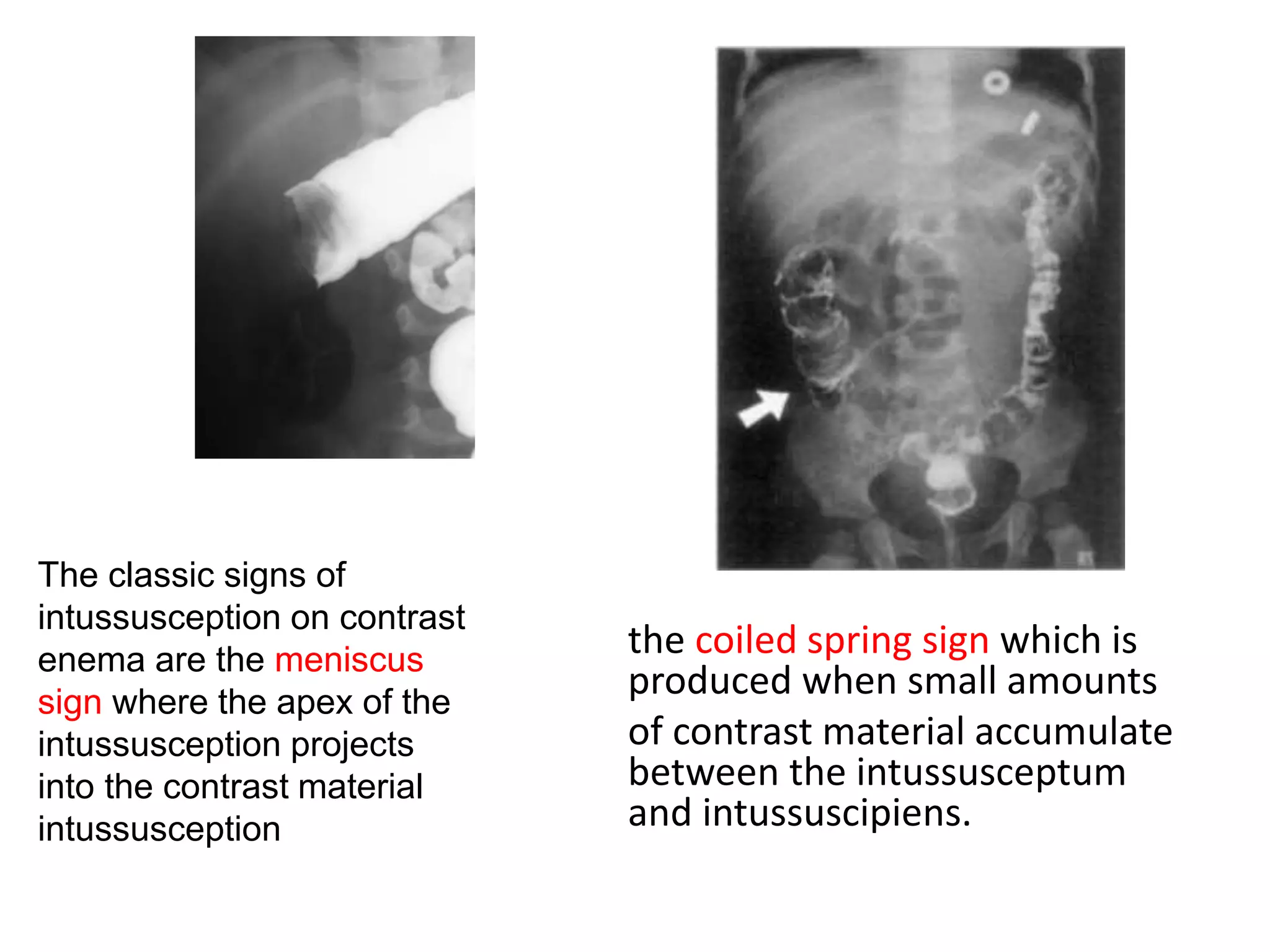
Intussusception is a condition where a segment of the bowel telescopes into another, most commonly seen in children aged between 3 months and 3 years. Clinical presentation includes intermittent abdominal pain, vomiting, and currant jelly stools, while diagnostic imaging can include ultrasound, CT scans, and contrast enemas. Treatment options range from non-operative reduction techniques with enemas to surgical intervention if complications arise.