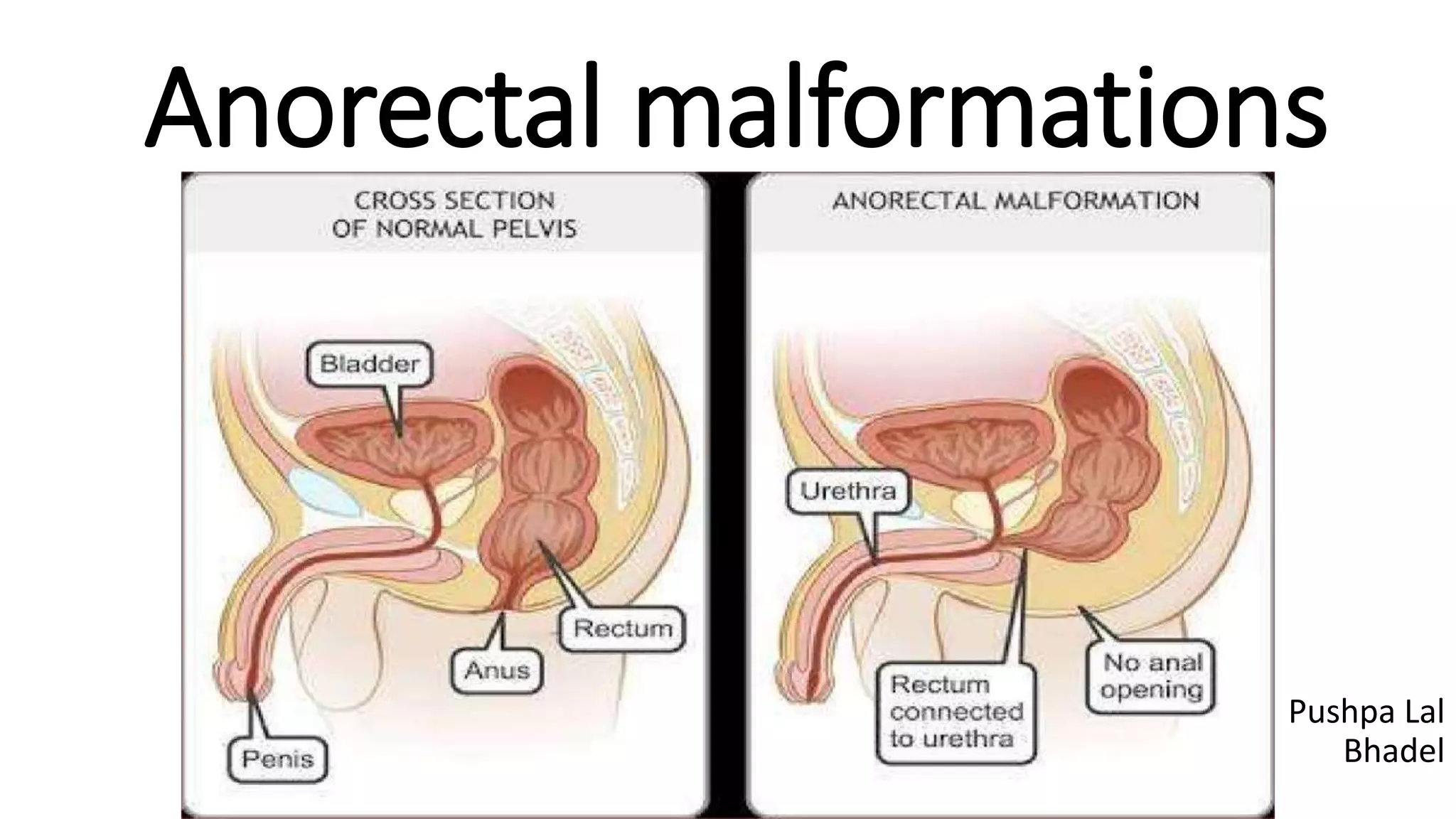
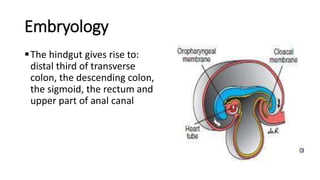
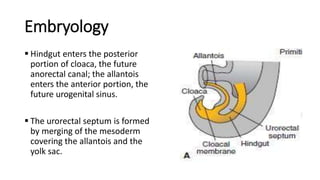
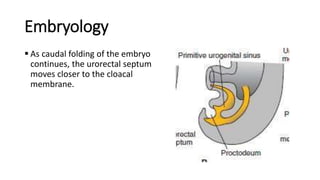
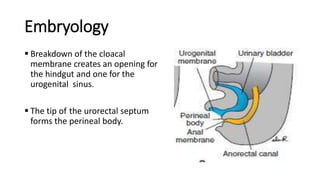
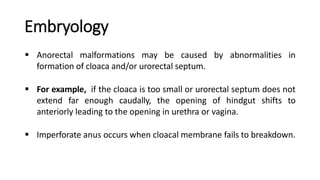
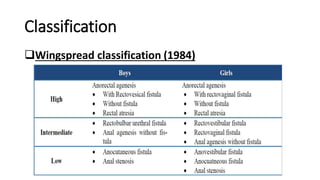
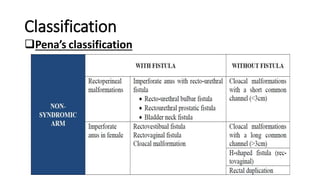
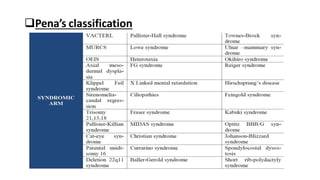
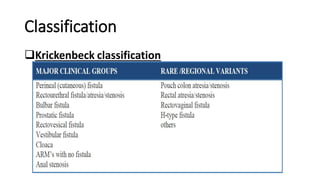
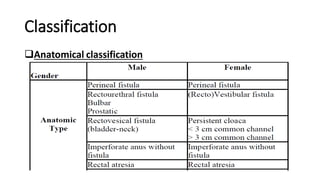
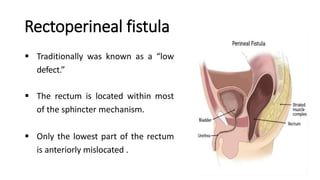
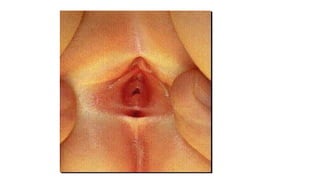
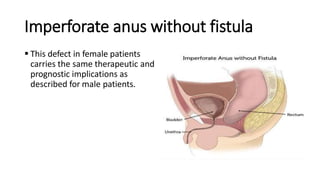
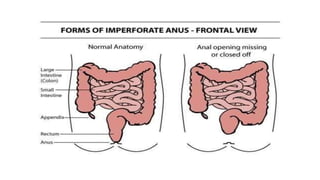
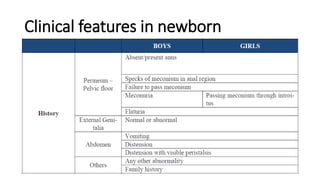
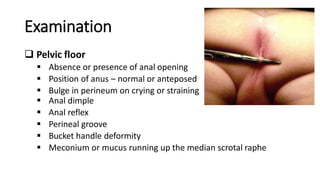
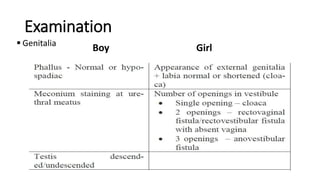
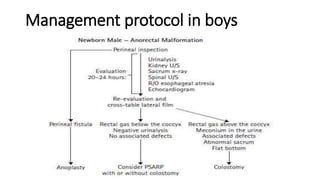
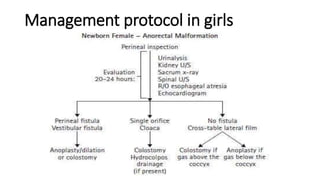
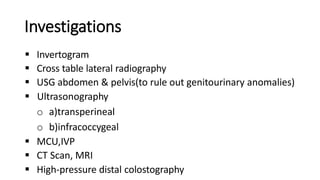
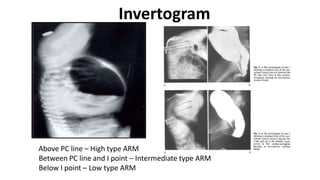
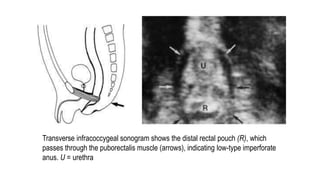
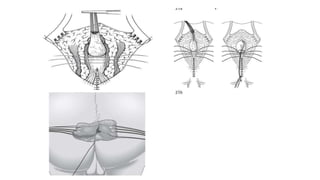
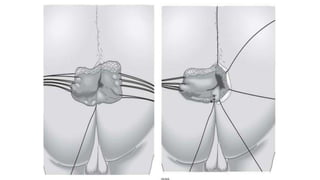
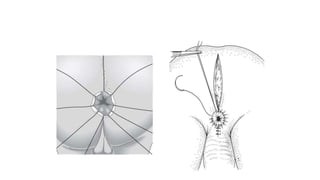
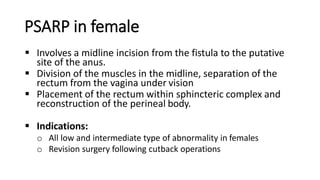
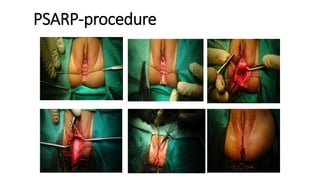
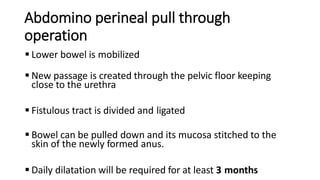
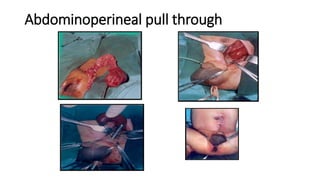
Anorectal malformations are birth defects where the anus and rectum do not develop properly. They occur in about 1 in 4,000 live births. The document discusses the various types of anorectal malformations including rectoperineal fistula, rectourethral fistula, and imperforate anus without fistula. It covers the embryology, classification systems, clinical features, investigations, and surgical management protocols for repairing defects in both male and female newborns. The posterior sagittal anorectoplasty technique is emphasized as the standard approach for repair.