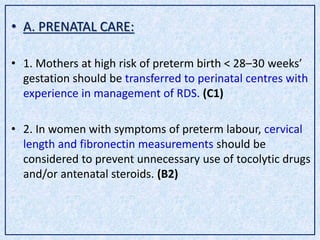
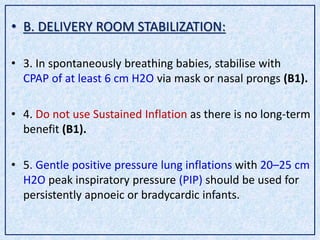
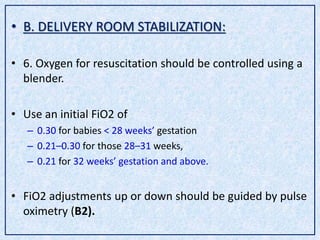
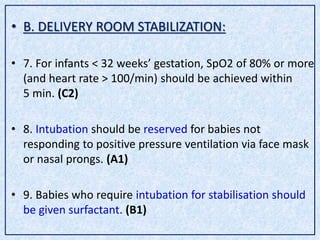
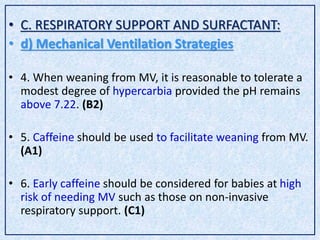
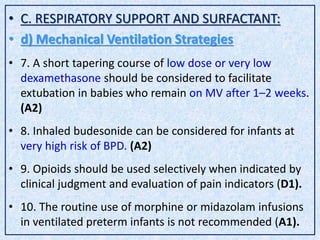
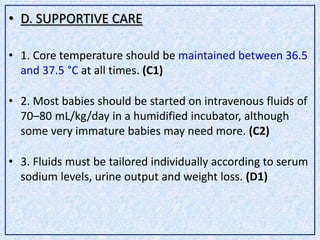
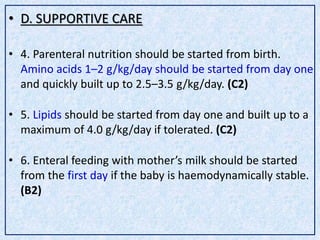
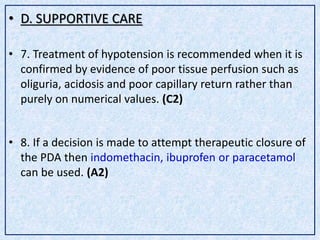
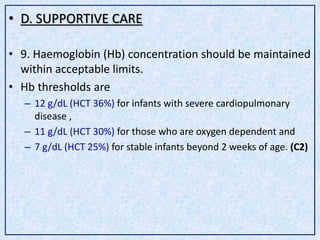
This document outlines the European consensus statement on respiratory distress syndrome (RDS) management from 2019. It provides recommendations on prenatal care, delivery room stabilization, respiratory support and surfactant therapy, and supportive care. The overall aims of RDS management are to maximize survival while minimizing adverse effects such as bronchopulmonary dysplasia. Key recommendations include prenatal corticosteroid administration, delayed cord clamping, use of continuous positive airway pressure and early rescue surfactant therapy. The consensus statement provides guidance on various respiratory support strategies, ventilation techniques, and supportive measures to optimize outcomes for infants with RDS.