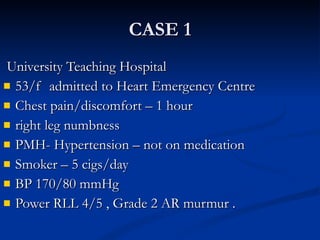
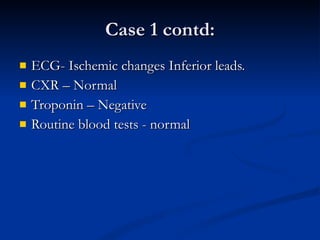
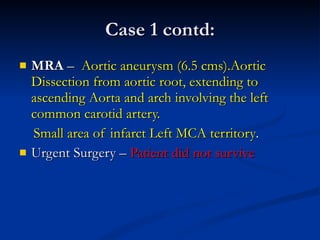
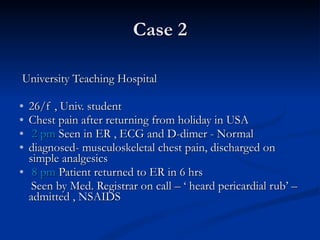
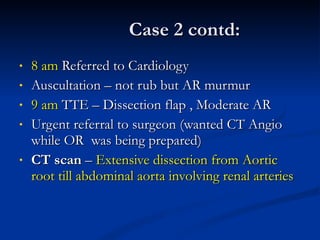
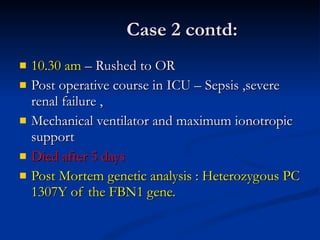
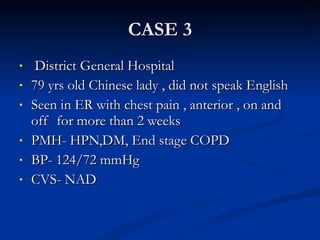
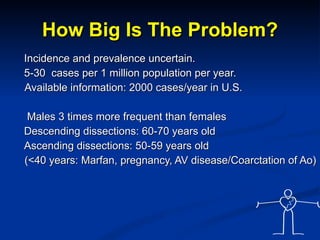
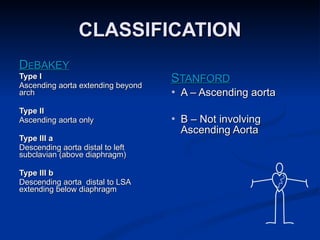
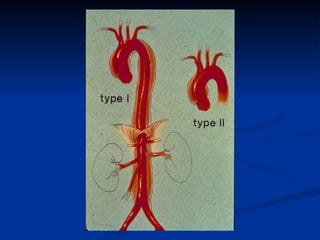
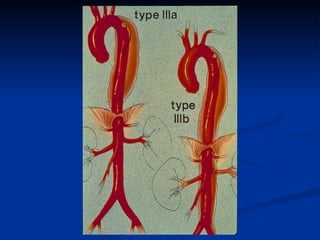
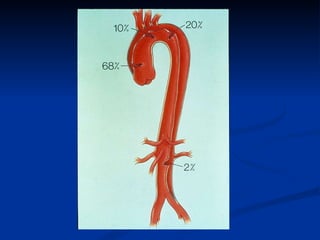
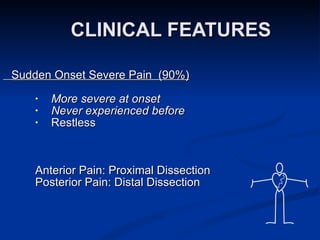
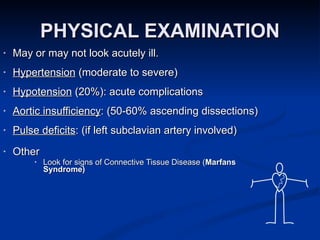
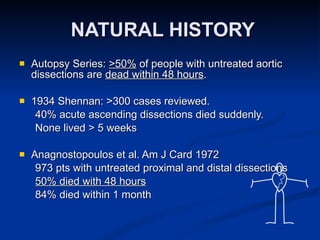
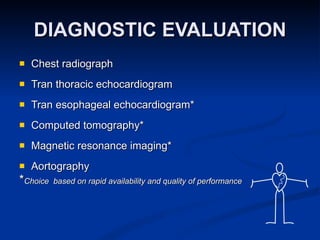
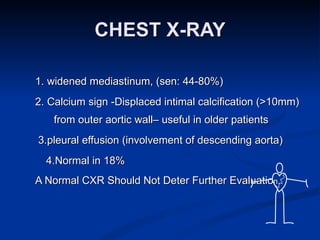
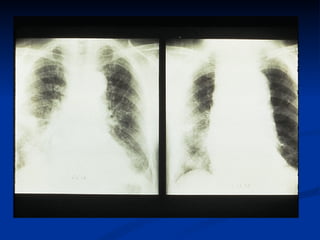
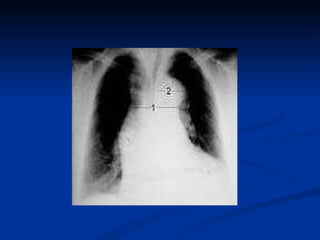
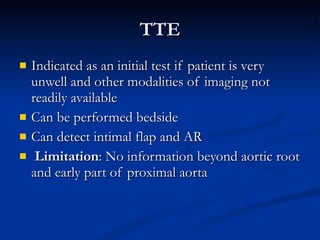
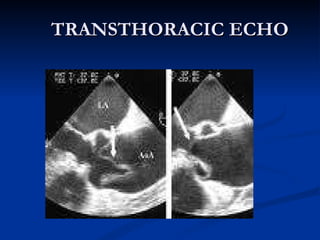
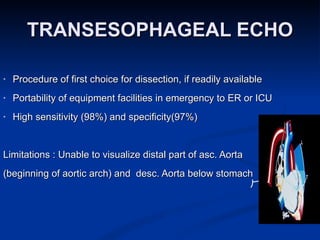
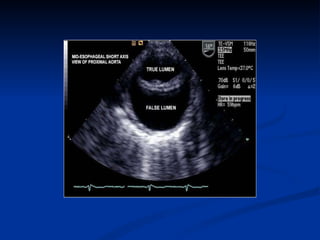
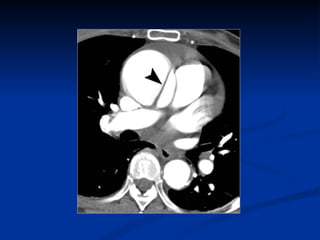
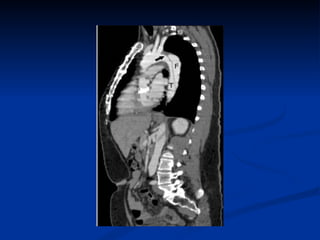
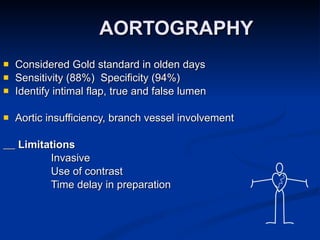
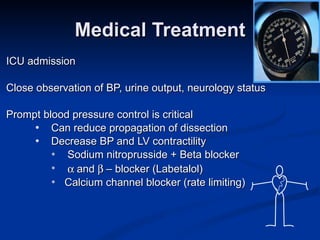
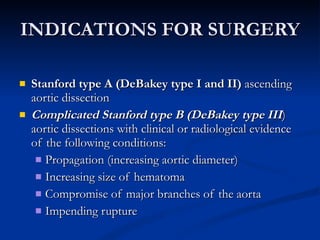
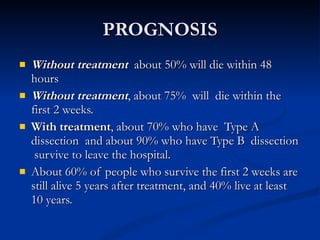
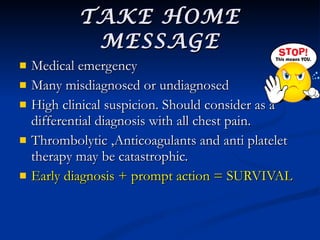
The document presents three case studies of aortic dissection, highlighting the critical importance of early recognition, diagnosis, and management to improve survival rates. It discusses the various clinical presentations and complications associated with aortic dissection, as well as the diagnostic imaging options and surgical versus medical management approaches. It emphasizes that a high clinical suspicion is essential due to the high mortality rates associated with untreated cases and underscores the need for immediate action in cases of suspected aortic dissection.