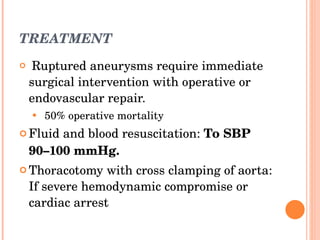
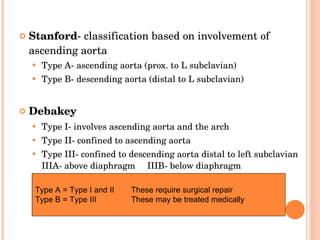
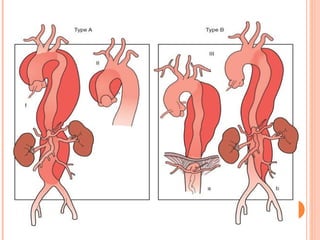
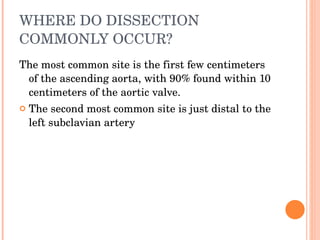
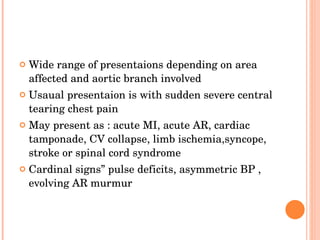
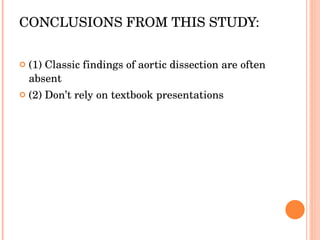
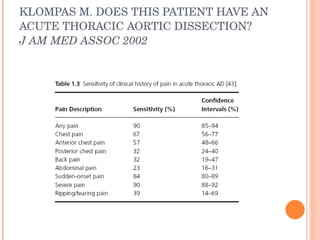
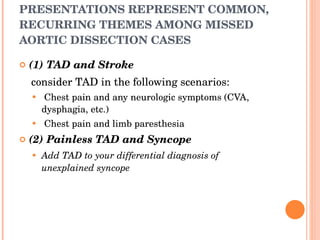
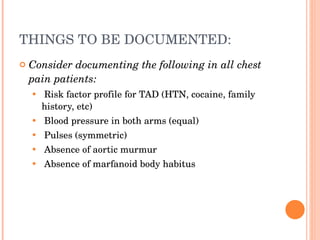
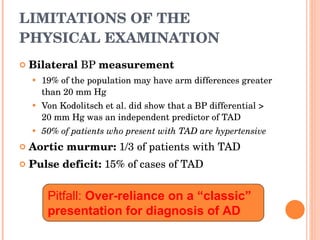
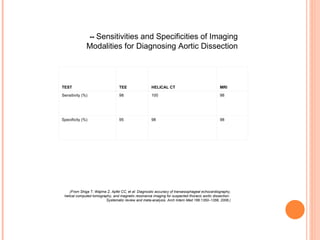
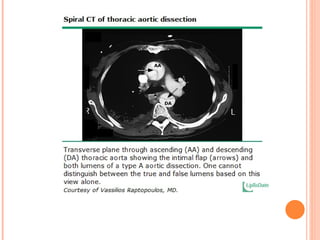
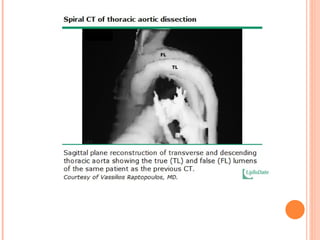
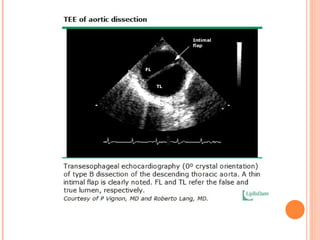
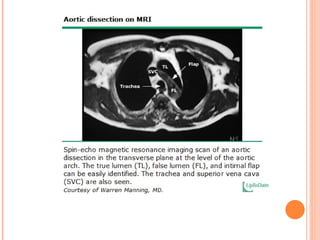
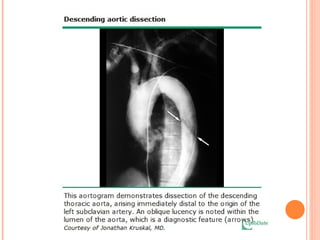
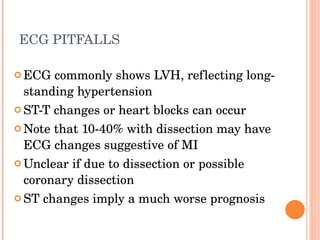
This document discusses aortic aneurysms and dissections. It covers risk factors, clinical presentations, diagnostic imaging and treatment. Key points include: thoracic aortic dissections have high mortality if undiagnosed; imaging modalities like CT, MRI and TEE are useful for diagnosis but presentations can be atypical; hypertension is a major risk factor; pain is the most common symptom but neurological symptoms, syncope or abdominal pain may occur instead.
![DEFINITIONS AND ANATOMY AND CLASSIFICATION SYSTEMS aorta is composed of three layers Aortic dissection occurs when ........ Classification Stanford DeBakey acute Vs chronic [ chronic if> 2 wks]](https://image.slidesharecdn.com/aorticdisasters-ahmed-101013005639-phpapp02/85/Aortic-disasters-ahmed-5-320.jpg)

![Characteristics of Aortic Dissection from the International Registry of Acute Aortic Dissection [4] LEFT VENTRICULAR HYPERTROPHY (%) ISCHEMIA (%) NORMAL ECG (%) WIDENED MEDIASTINUM ON CXR (%) NORMAL CXR (%) PULSE DEFICIT (%) AORTIC INSUFFICiENCY MURMUR (%) SYNCOPE (%) CHEST PAIN (%) 26 15 31 62 12 15 32 9 73 All ( n = 464) 25 17 31 63 11 19 44 13 79 Type A ( n = 289) 32 13 32 56 16 9 12 4 63 Type B ( n = 175)](https://image.slidesharecdn.com/aorticdisasters-ahmed-101013005639-phpapp02/85/Aortic-disasters-ahmed-17-320.jpg)



![Table 84-1 -- Prevalence of Abdominal Aortic Aneurysms (AAAs) in Selected Risk Groups INCIDENCE (%) GROUP 2–4 Autopsy subjects aged 50 years or old 5,6] 5–10 Men aged 65 years or older [4,7] 10–15 Patients with coronary artery disease [8] or occlusive peripheral vascular disease [9,10] 20–30 Brothers of patients with AAAs [11,12]](https://image.slidesharecdn.com/aorticdisasters-ahmed-101013005639-phpapp02/85/Aortic-disasters-ahmed-57-320.jpg)
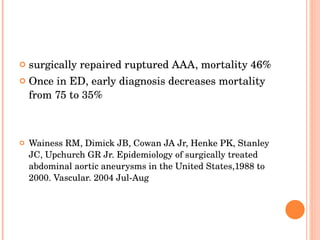
![SYMPTOMS ■ Most aneurysms are asymptomatic when discovered (60-80%)and become symptomatic when expanding or ruptured. ■ Acute pain in abdomen, back, or flank [ 75% ] ■ Nausea and vomiting ■ Syncope or near syncope urologic symptoms 10%](https://image.slidesharecdn.com/aorticdisasters-ahmed-101013005639-phpapp02/85/Aortic-disasters-ahmed-58-320.jpg)
![EXAM ■ Vital signs may be surprisingly normal. ■ Hypotension and shock if rupture with significant blood loss ■ Abdominal tenderness, distension, or pulsatile abdominal mass [75% above umbilicus] ■ Evidence for retroperitoneal hematoma ■ Periumbilical ecchymosis ( Cullen’s sign) ■ Flank ecchymosis ( Grey-Turner’s sign) ■ Massive GI bleed if rupture into GI tract (aortoenteric fistula) ■ High-output heart failure if rupture into vena cava (aortocaval fistula)](https://image.slidesharecdn.com/aorticdisasters-ahmed-101013005639-phpapp02/85/Aortic-disasters-ahmed-59-320.jpg)