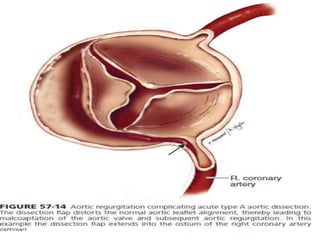
An aortic dissection is a tear in the inner layer of the aorta that allows blood to flow between the layers of the aortic wall, creating a false passageway. It is a medical emergency that requires prompt diagnosis and treatment. Type A dissections, which involve the ascending aorta, require emergency surgery while type B dissections, involving only the descending aorta, are generally treated medically with blood pressure control. Surgical treatment of type A dissections aims to remove the damaged aortic segment and restore blood flow through the aorta using a graft.