This document discusses aortic dissection, including:
1. It provides an introduction defining acute aortic syndromes and the types of aortic dissection.
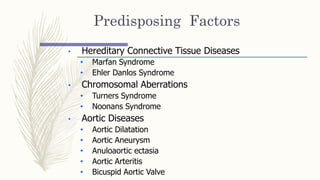
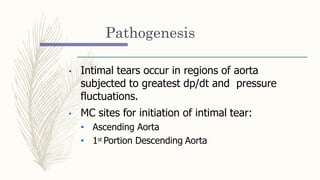
2. It covers the incidence, risk factors, classifications, pathogenesis, natural history, signs and symptoms, diagnostic testing including imaging and labs, and management approaches for aortic dissection.
3. The management focuses on reducing blood pressure and pulse pressure through beta blockers and other antihypertensive drugs to prevent extension of the dissection.