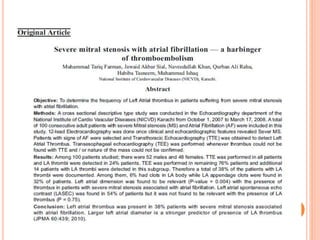
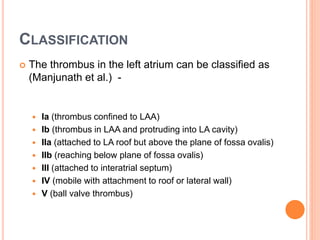
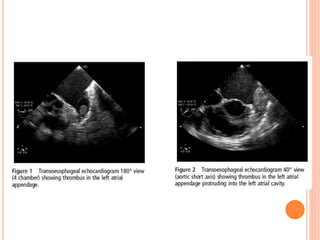
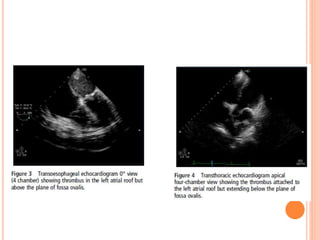
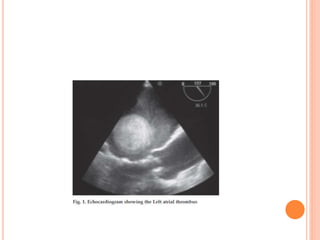
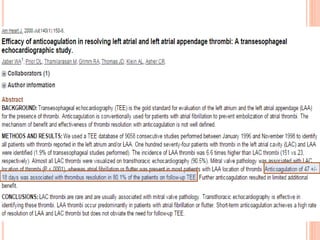
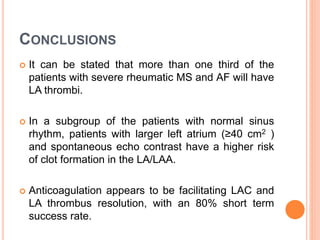
This document discusses left atrial thrombus in patients with rheumatic mitral stenosis. It finds that 26-33% of patients with severe mitral stenosis have left atrial thrombi, which are associated with a higher risk of embolic events. The document classifies different types of left atrial thrombi and examines determinants of thrombus formation like atrial fibrillation, left atrial size, and severity of mitral stenosis. It recommends anticoagulation to reduce thromboembolic risk, noting studies have found anticoagulation facilitates thrombus resolution.