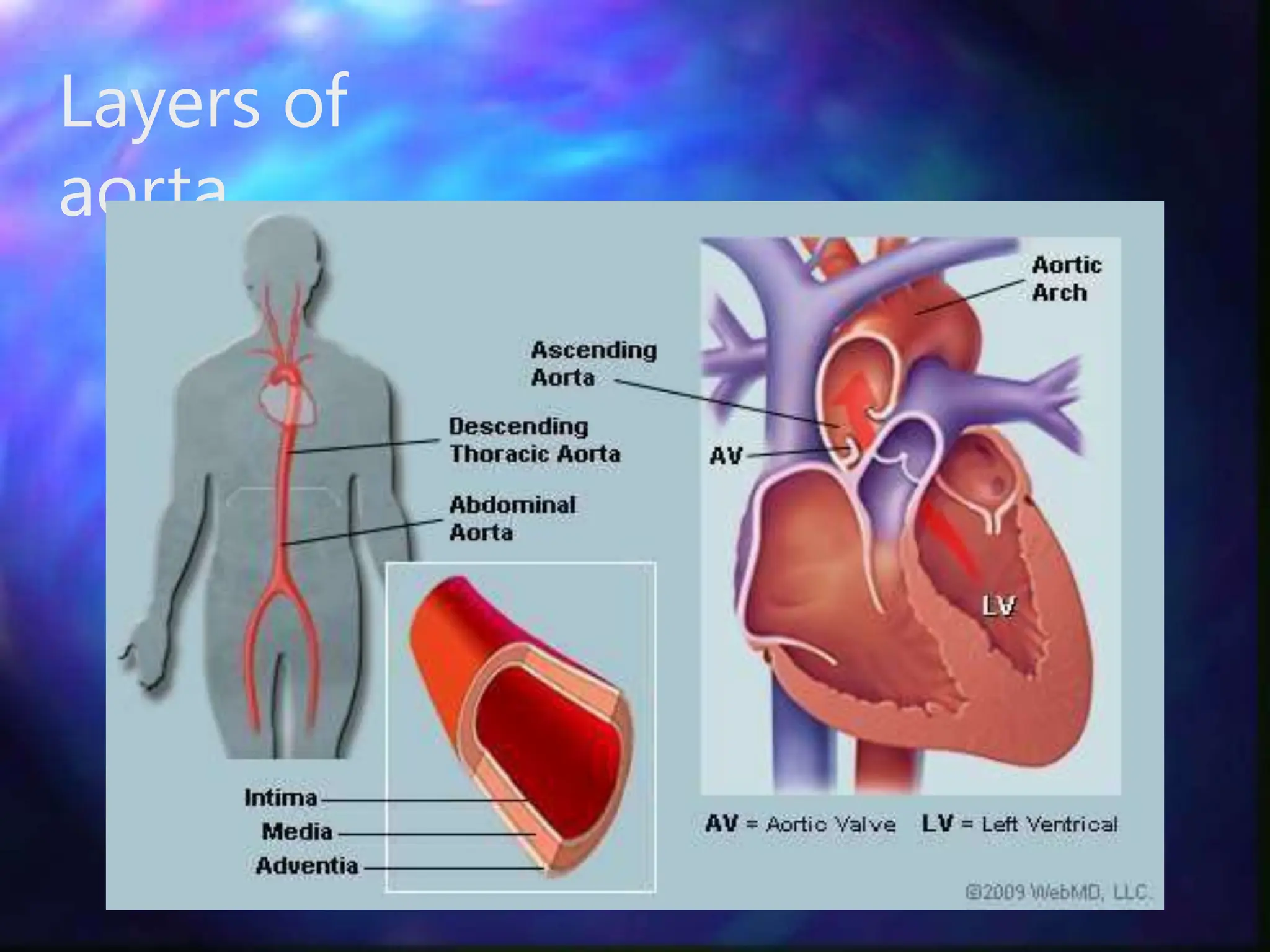
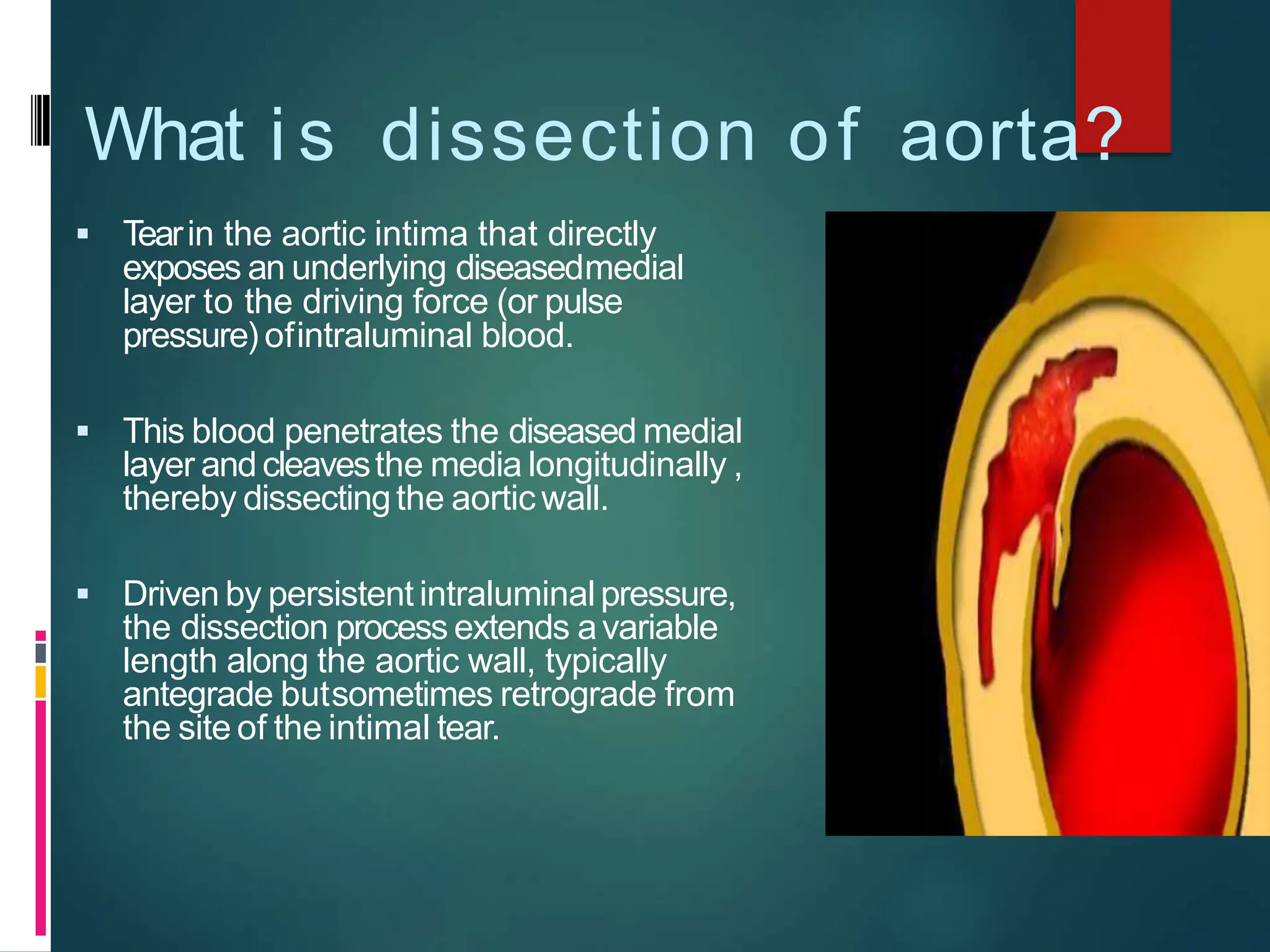
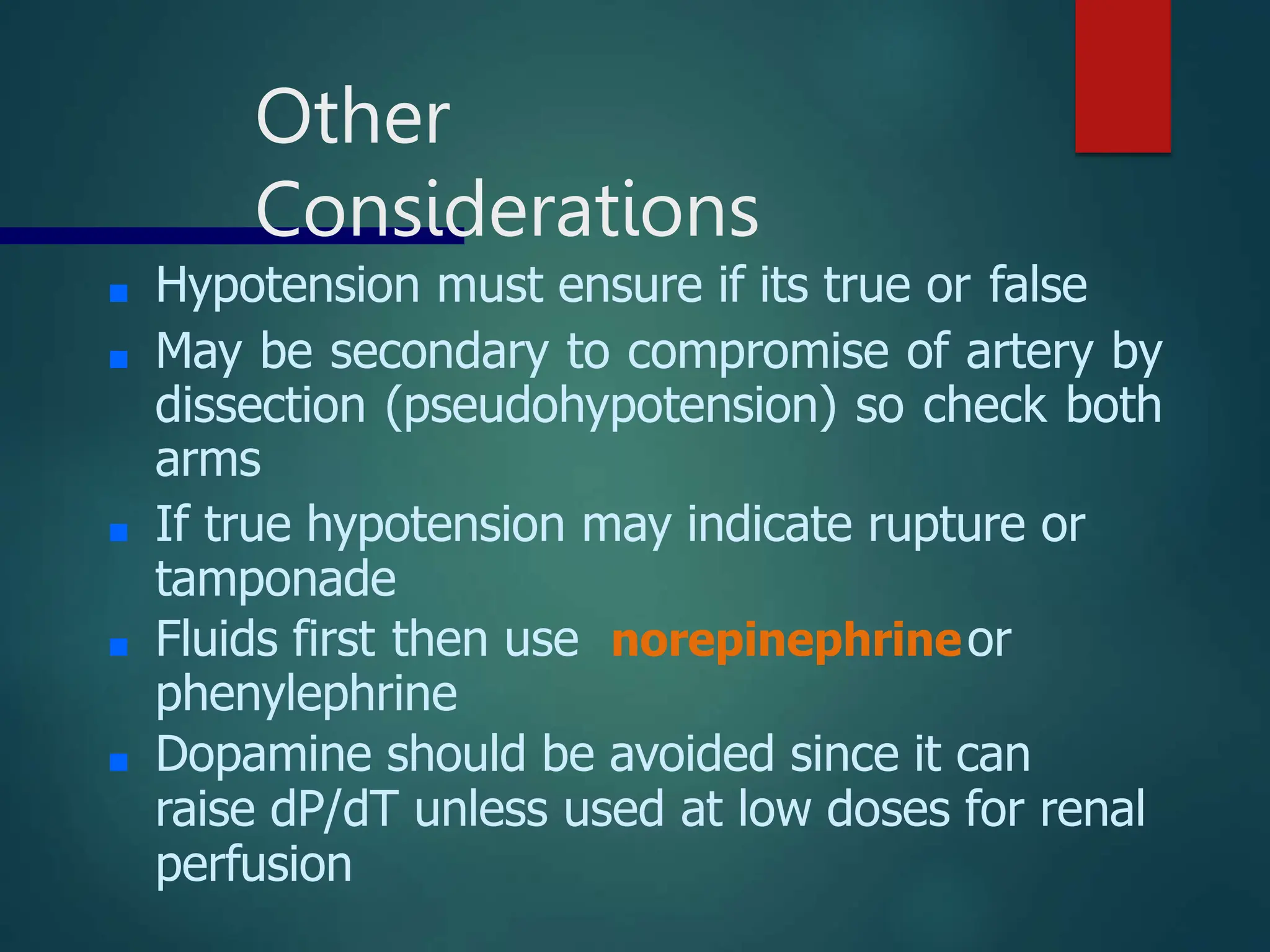
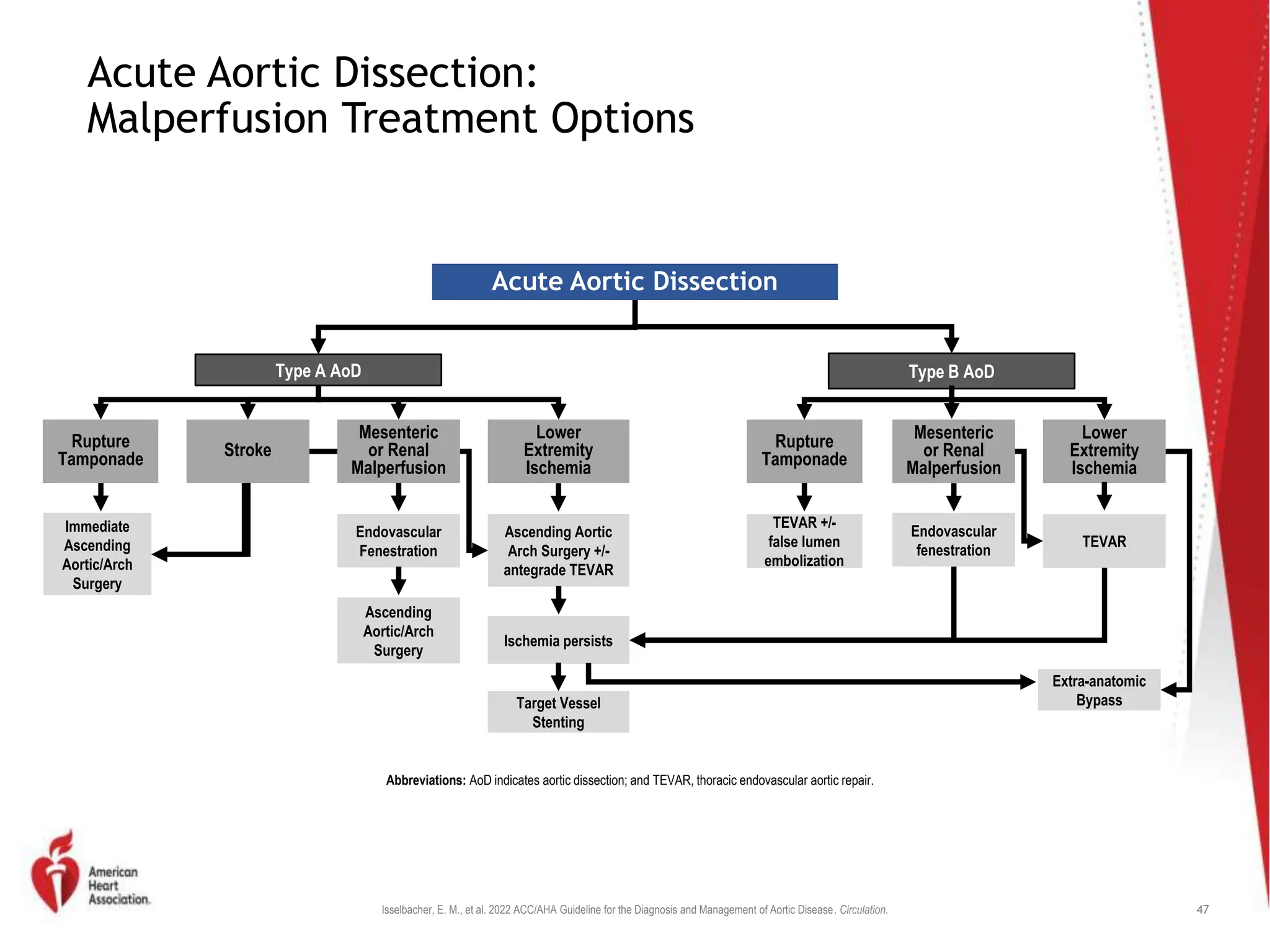
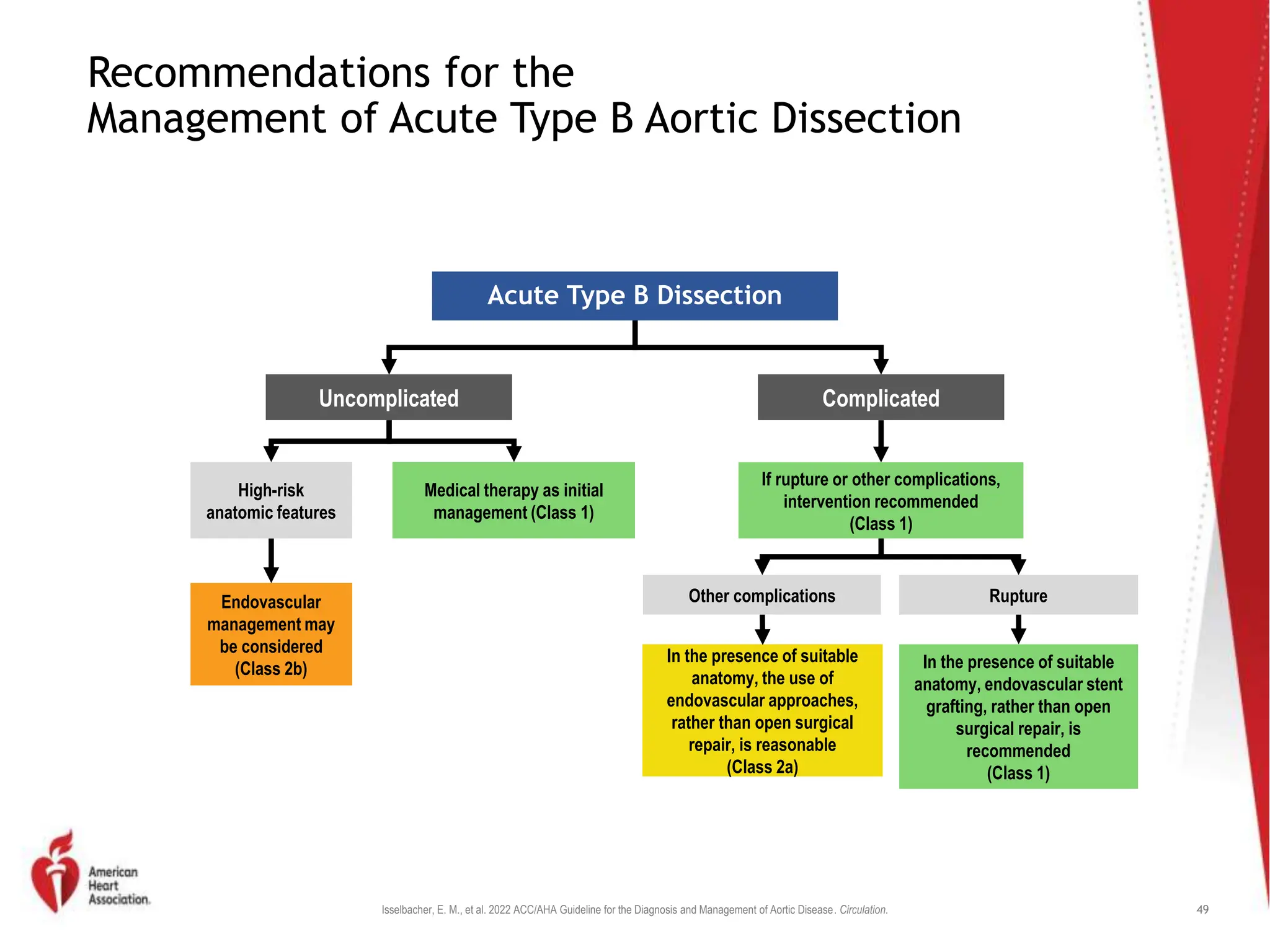
Aortic emergencies are life-threatening conditions involving the aorta that require timely diagnosis and management. Aortic dissection, a tear in the aortic wall that causes blood to flow abnormally within the wall, is a common aortic emergency. It is usually caused by high blood pressure damaging the aortic wall. Symptoms include a sudden, severe chest pain and pulse abnormalities. Diagnosis involves imaging tests like CT, MRI, or angiography. Treatment aims to lower blood pressure and heart contractility to prevent dissection progression, often using beta blockers. Surgery is usually recommended for type A dissections involving the ascending aorta, while type B dissections of the descending aorta may be treated medically or