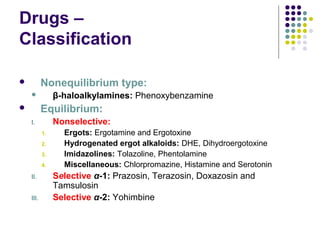
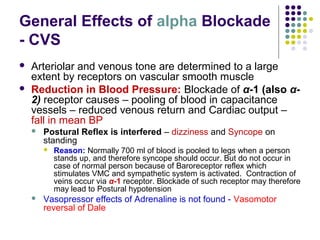
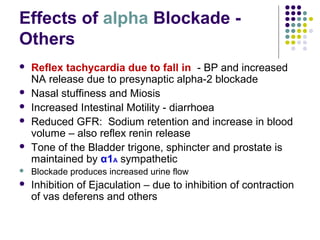
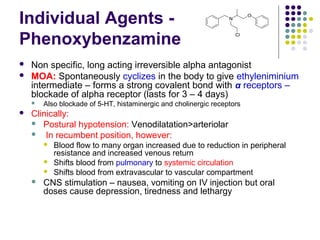
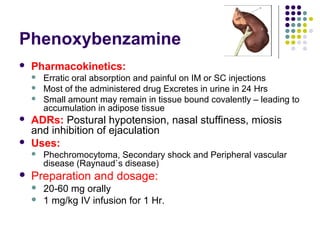
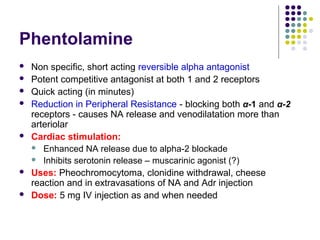
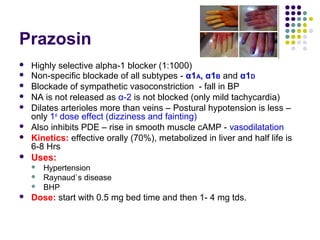
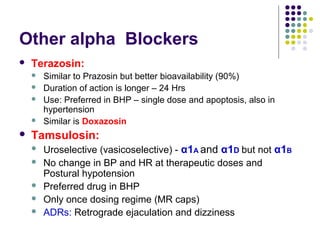
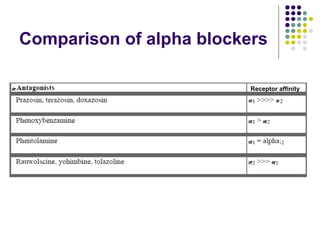
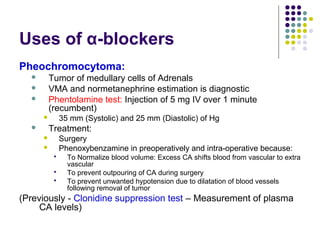
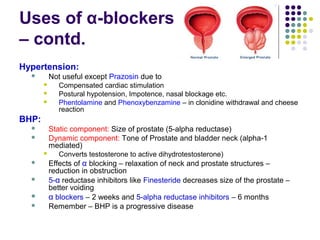
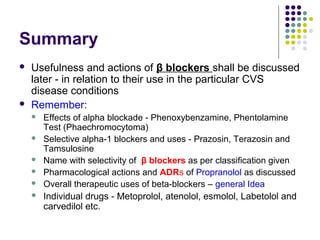
Antiadrenergic drugs, also known as alpha blockers or alpha antagonists, work by blocking the effects of adrenaline and other related drugs at receptor sites. They occupy both alpha-1 and alpha-2 adrenergic receptors without activating them. Clinically, they are used to modify the responses of endogenous catecholamines like adrenaline and noradrenaline in both physiological and pathophysiological conditions. Common uses include treating pheochromocytoma, hypertension, Raynaud's disease, and benign prostatic hyperplasia. Individual drugs vary in their selectivity and duration of action at different receptor subtypes. Side effects may include postural hypotension, nasal congestion, and inhibition of ejac