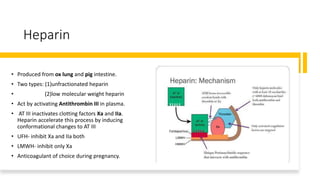
This document summarizes different types of anticoagulants, including their mechanisms of action, monitoring, and therapeutic uses. It discusses oral anticoagulants like warfarin that act by inhibiting vitamin K, as well as injectable anticoagulants like heparin and novel anticoagulants that directly inhibit coagulation factors. Warfarin is monitored using INR while heparin is monitored using aPTT or anti-Xa assay. Anticoagulants are used to treat conditions involving increased risk of blood clots like deep vein thrombosis, pulmonary embolism, atrial fibrillation, and ischemic stroke.