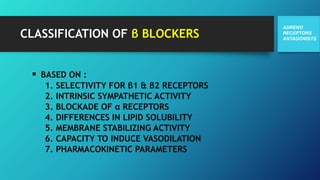
Beta blockers were first developed in the 1950s and propranolol was the first clinically useful beta blocker introduced in 1962 for treatment of angina. Beta blockers are classified based on selectivity for beta1/beta2 receptors and other properties. They are used clinically for cardiovascular conditions like hypertension, angina, arrhythmias, and heart failure as well as non-cardiac uses for conditions like migraine, anxiety, and glaucoma. Common side effects include fatigue, bronchospasm, hypoglycemia, and depression. Newer generations of beta blockers have additional properties like alpha-1 receptor blockade.