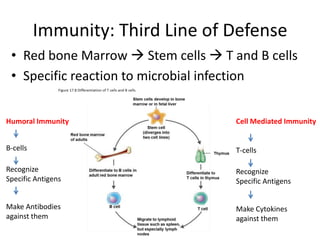
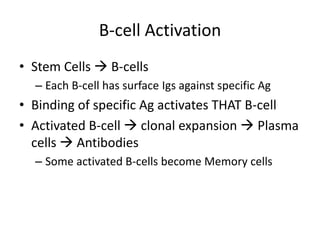
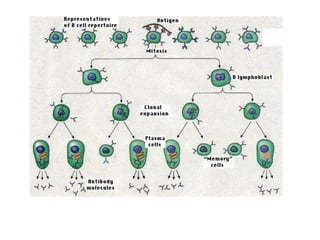
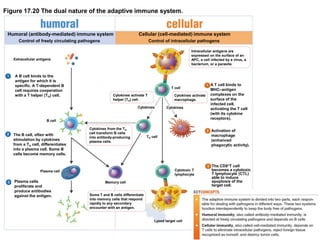
Adaptive immunity involves both humoral and cellular responses. B-cells produce antibodies that circulate in the blood and lymph to neutralize pathogens and toxins. T-cells recognize intracellular pathogens through antigen presentation and induce cytotoxic killing of infected cells. Antibodies and T-cells are activated through antigen recognition and work together to provide long-lasting adaptive immunity against specific pathogens. Vaccines utilize this immune memory to safely induce immunity against harmful diseases.






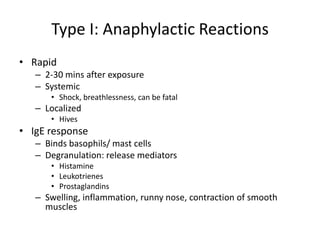
![Type III: Immune Complex Reactions
• IgG/ IgM against soluble antigens circulating in serum
Immune complexes:
• [Ag] > [Ab]
• Complexes evade phagocytes
• Soluble, circulating
• “stuck” on capillaries, joints, organ tissues
• Activate complement:
Transient Inflammation
Attract neutrophils enzymes
- tissue destruction
Glumerulonephritis = inflammatory
damage to kidney glomeruli](https://image.slidesharecdn.com/adaptiveimmunity-140409143247-phpapp01/85/11-Adaptive-Immunity-53-320.jpg)