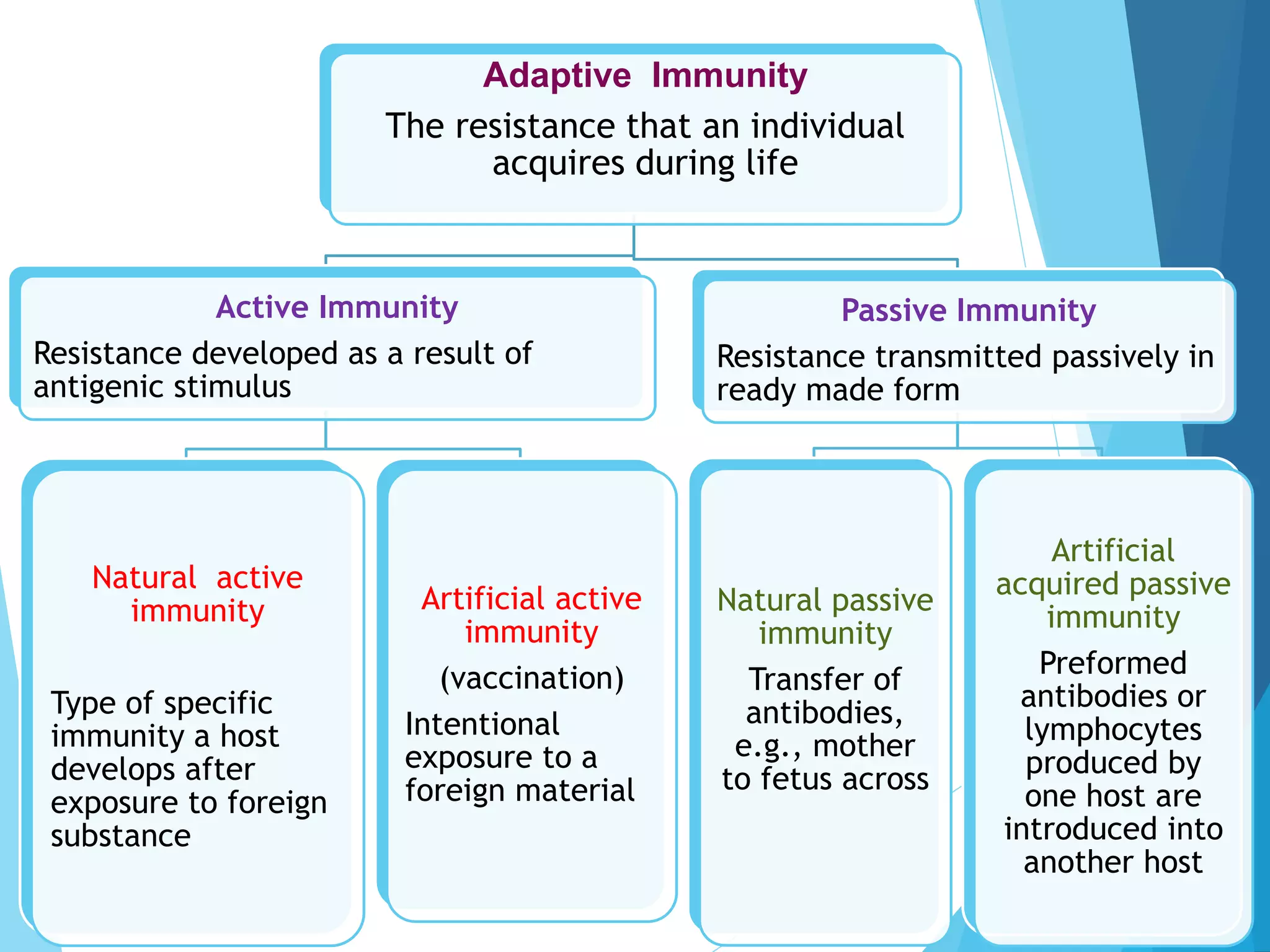
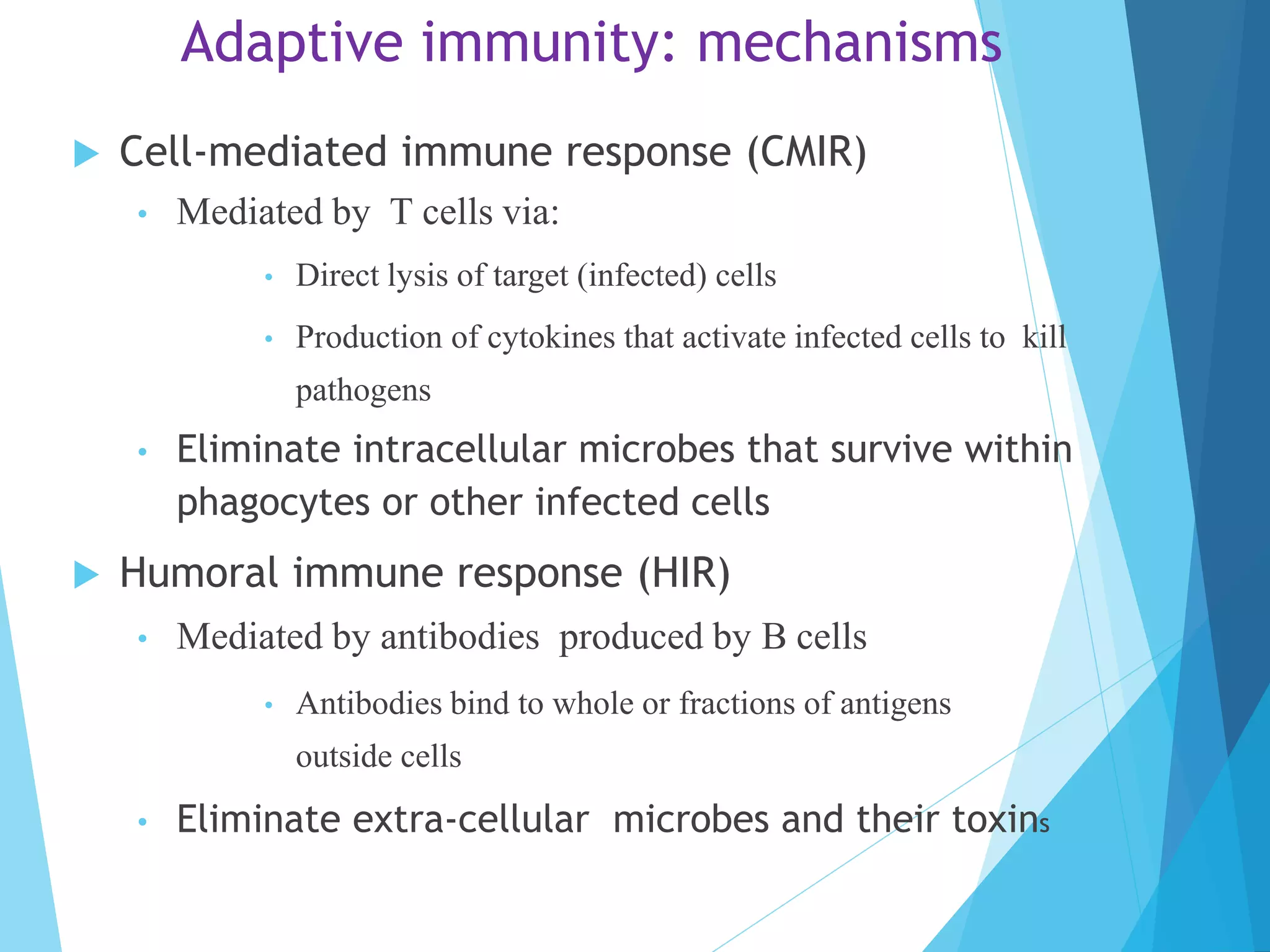
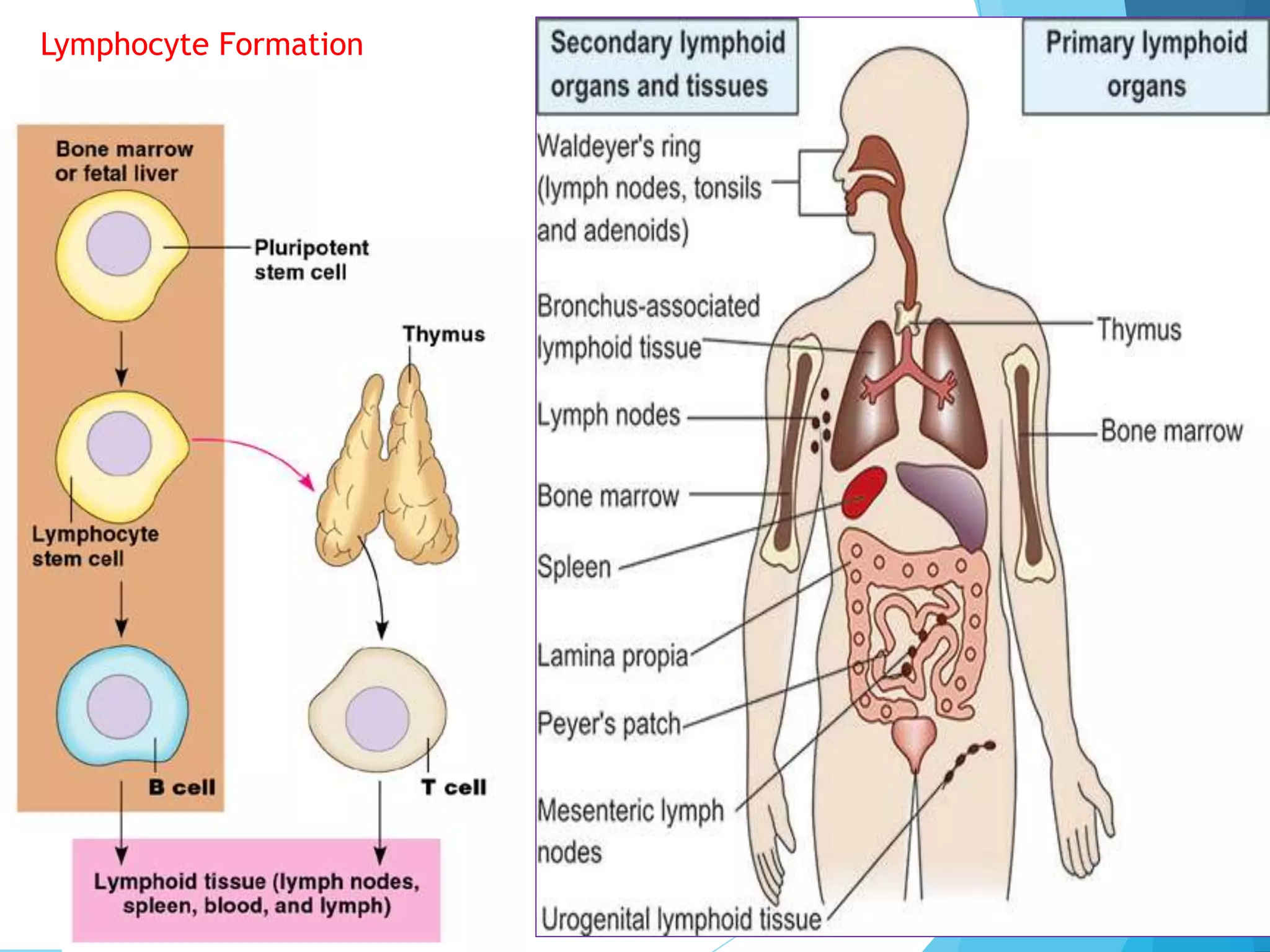
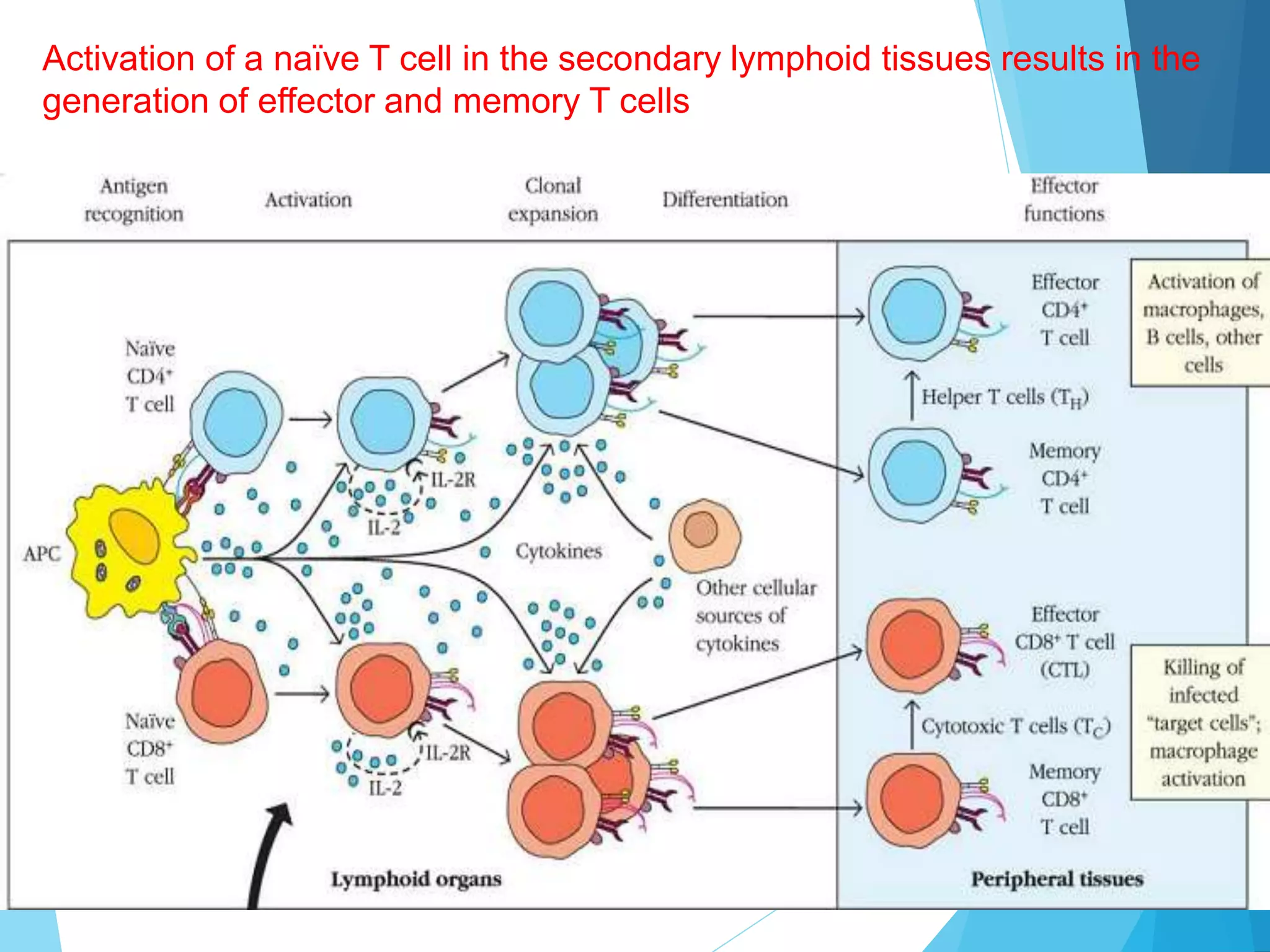
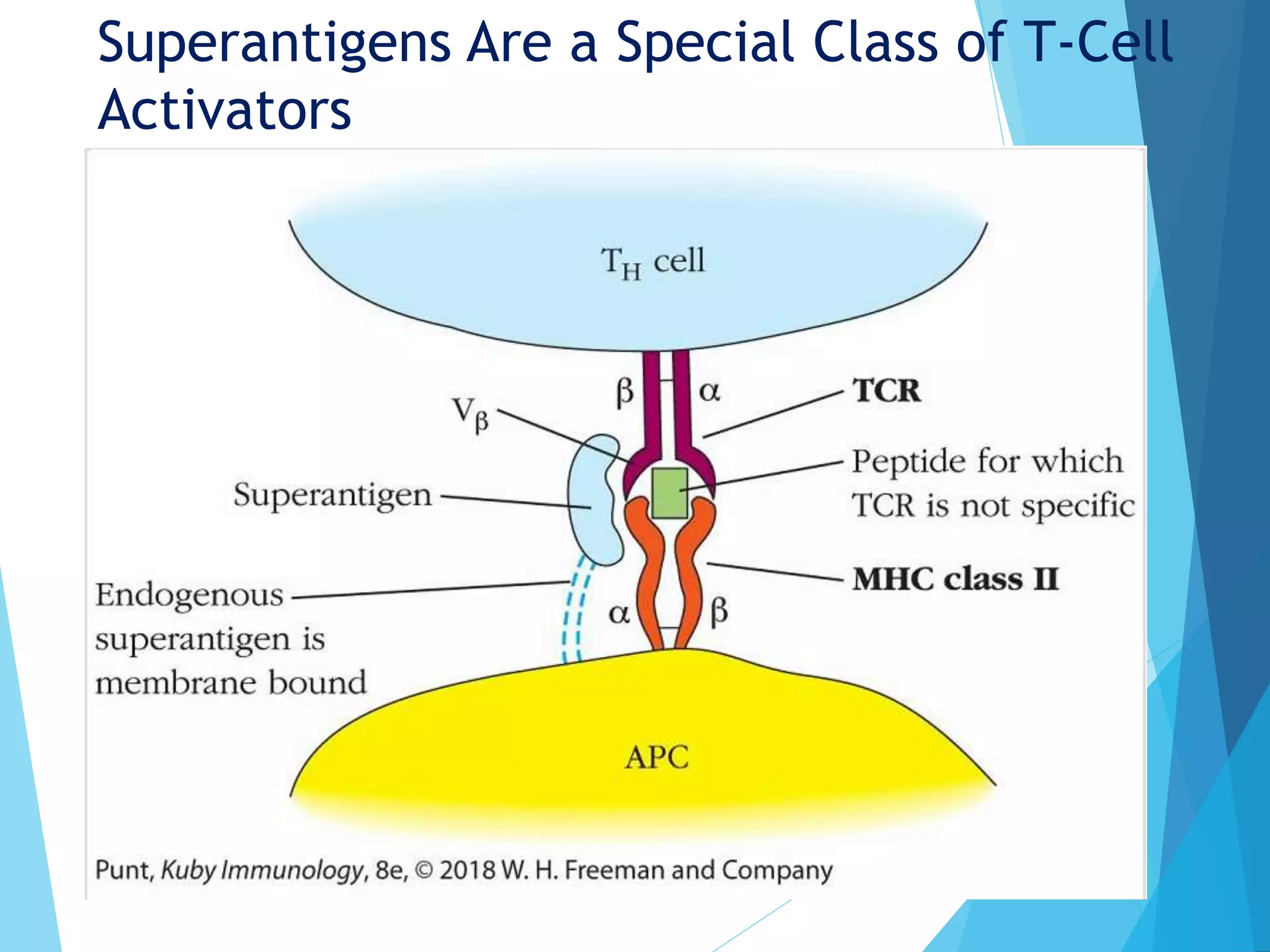
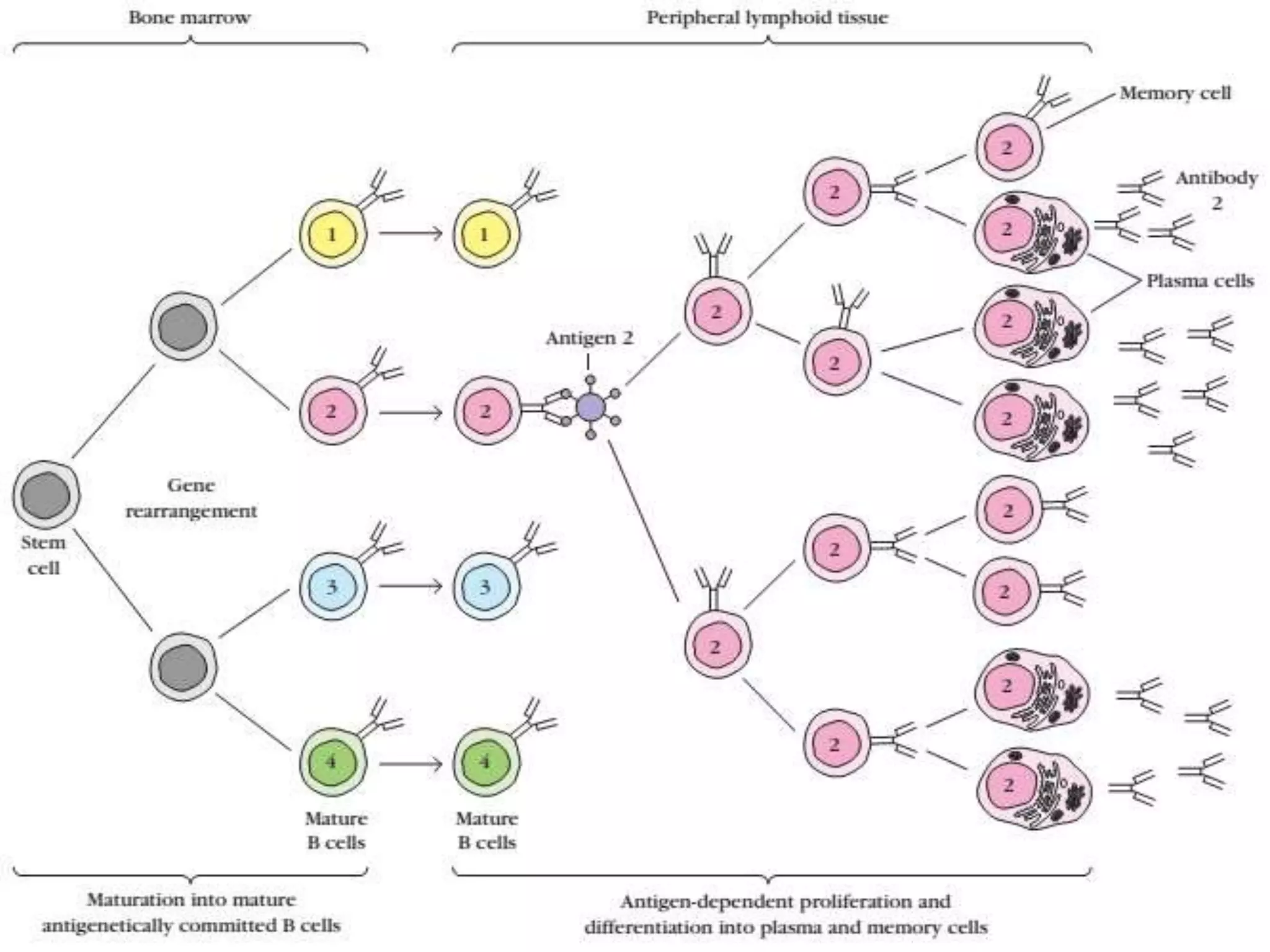
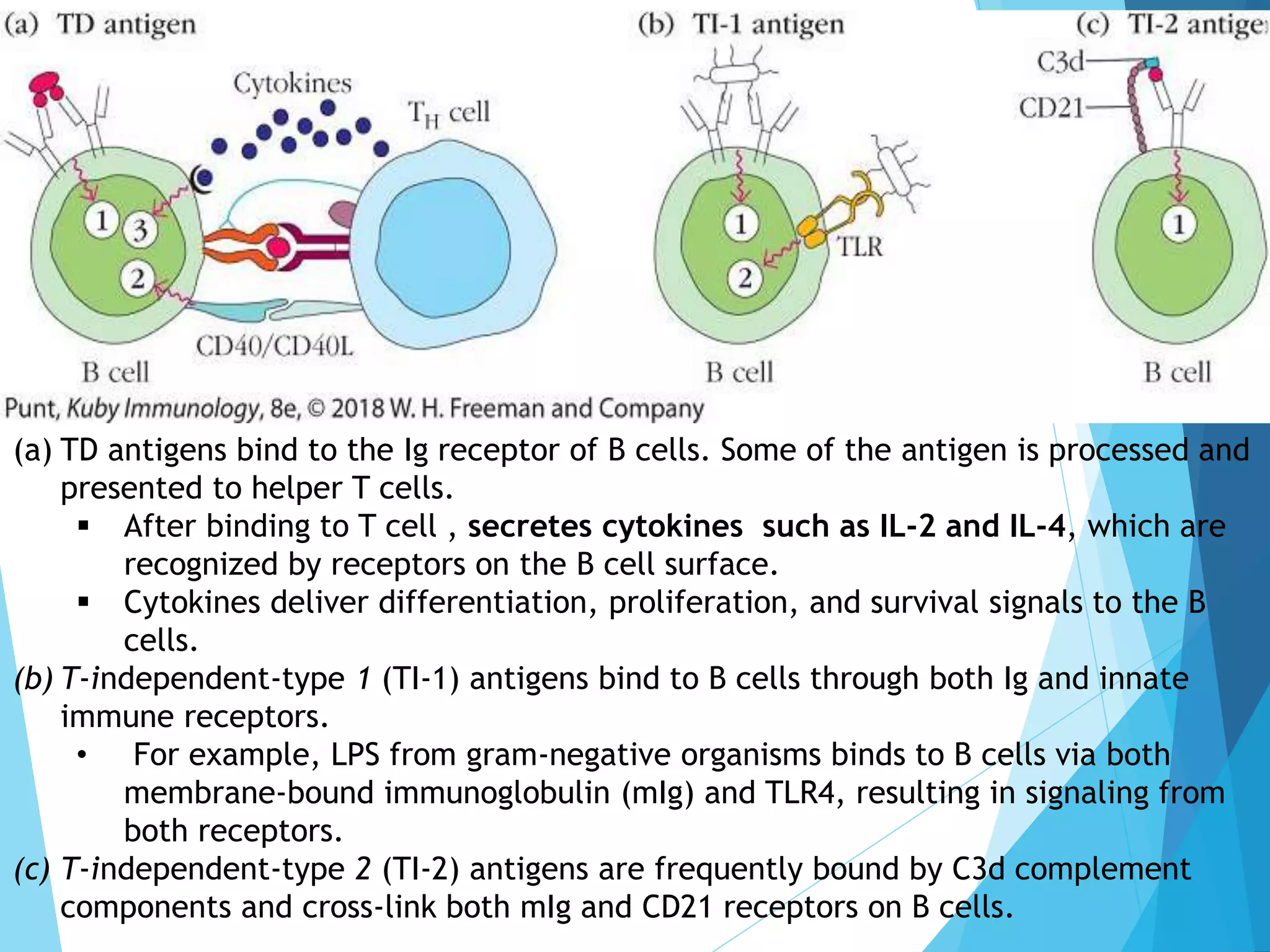
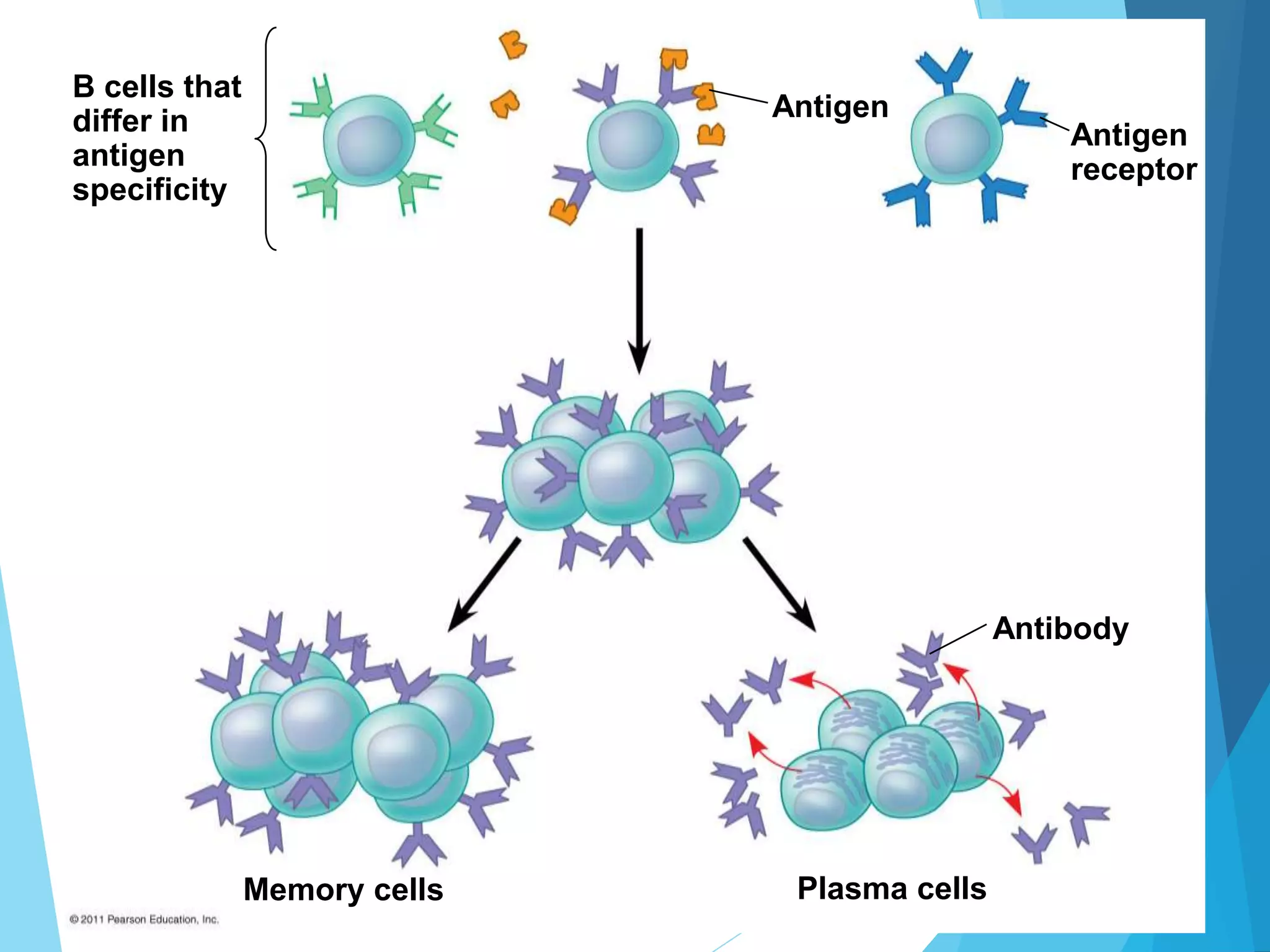
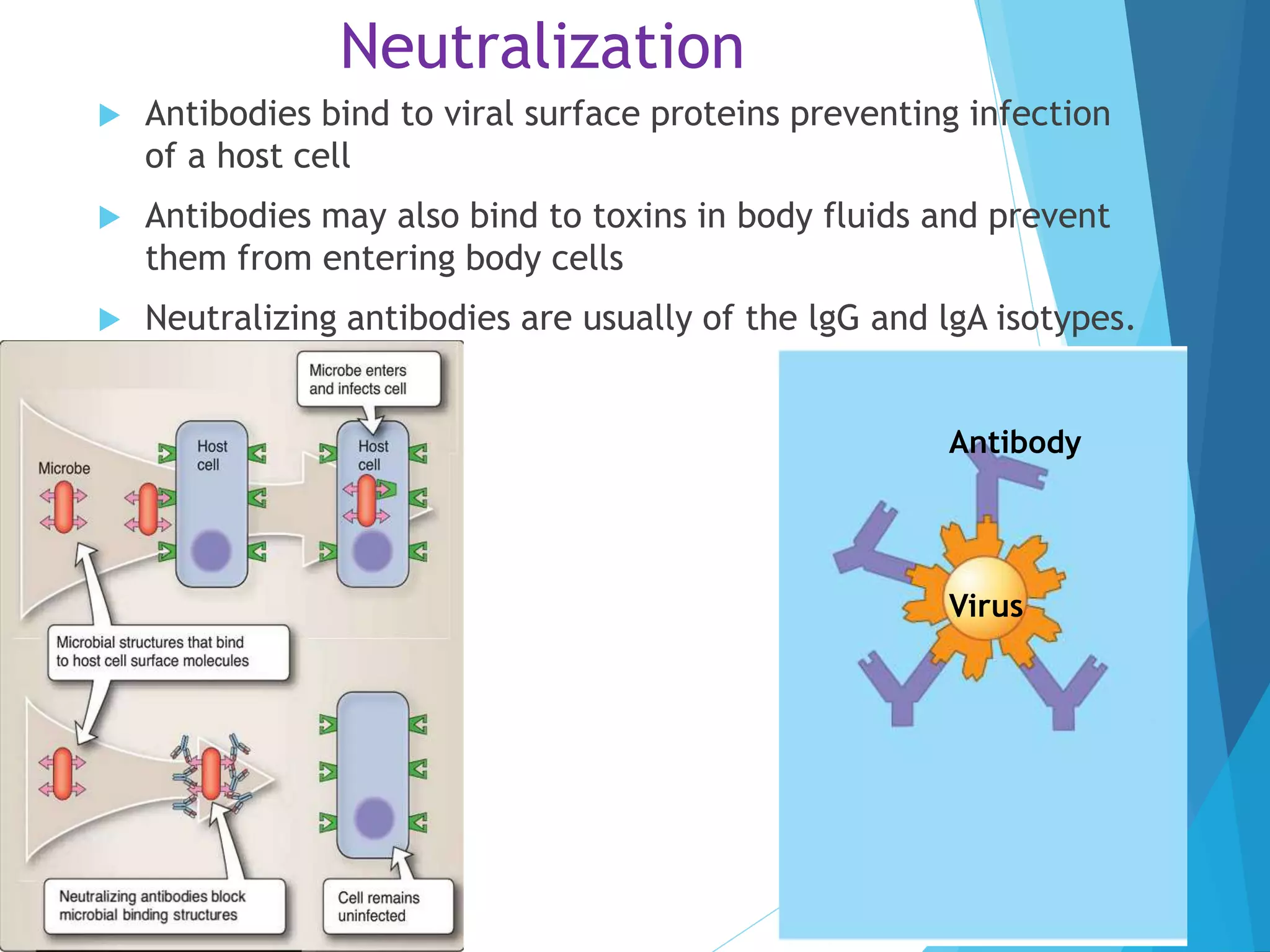
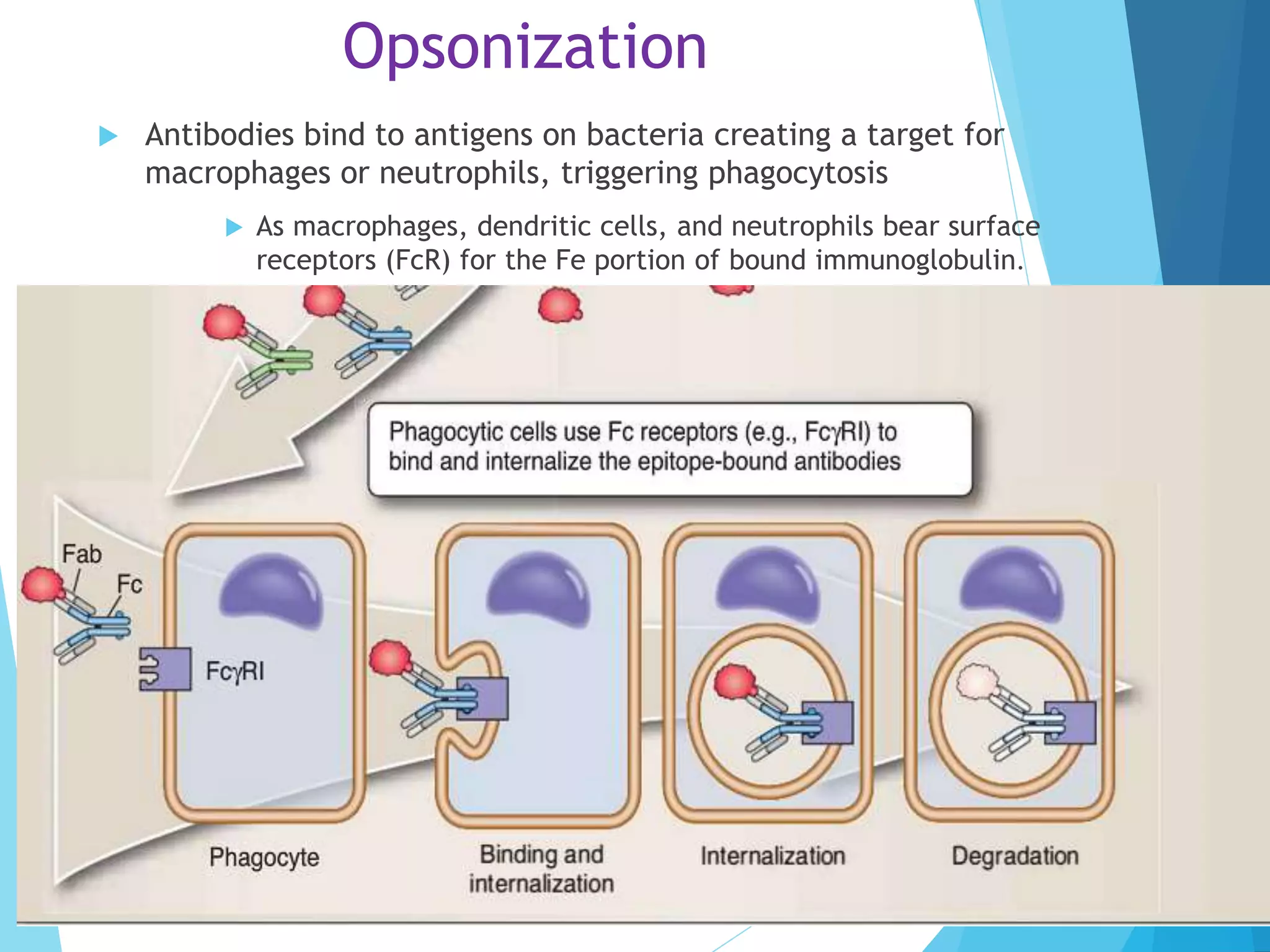
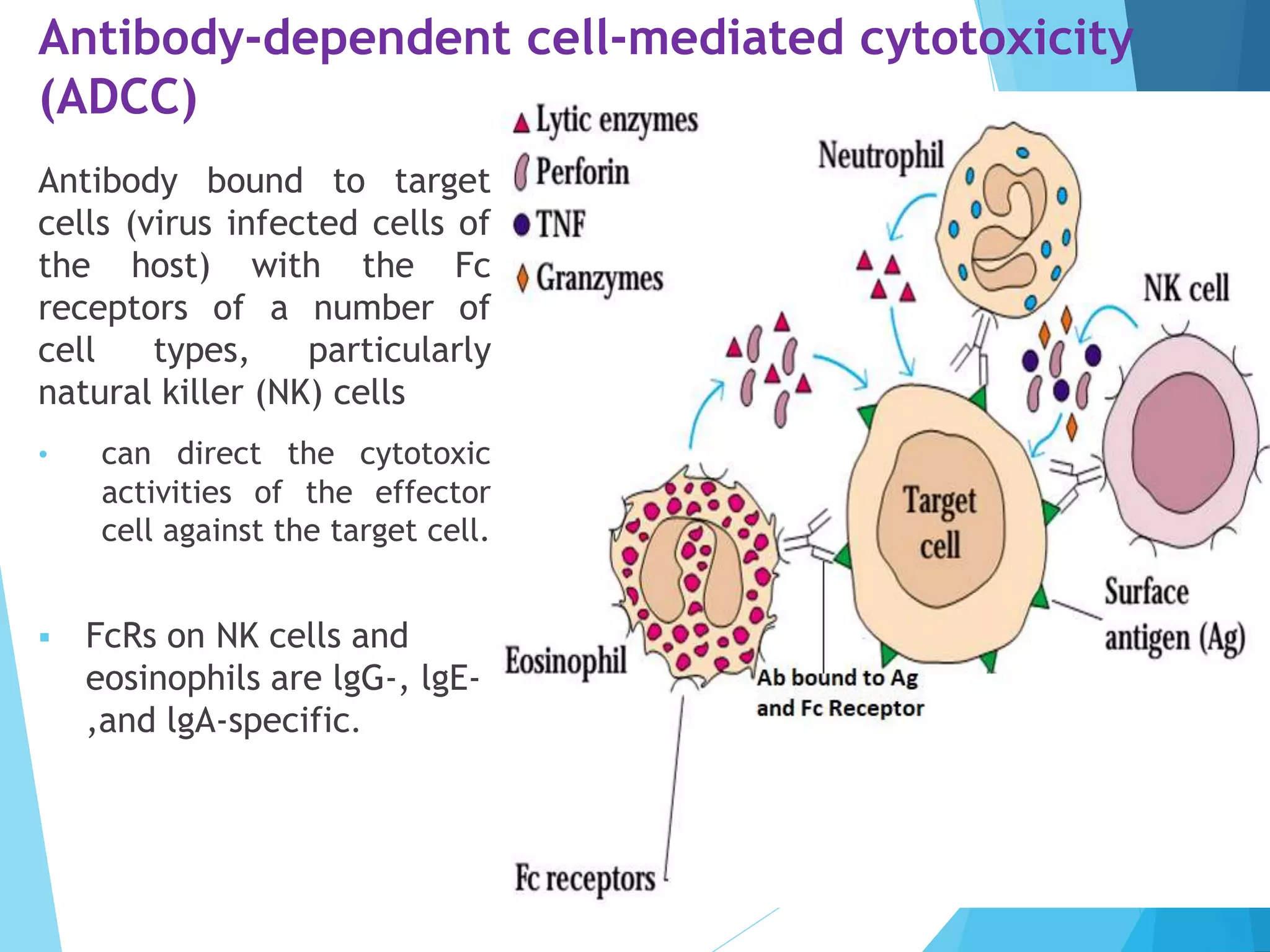
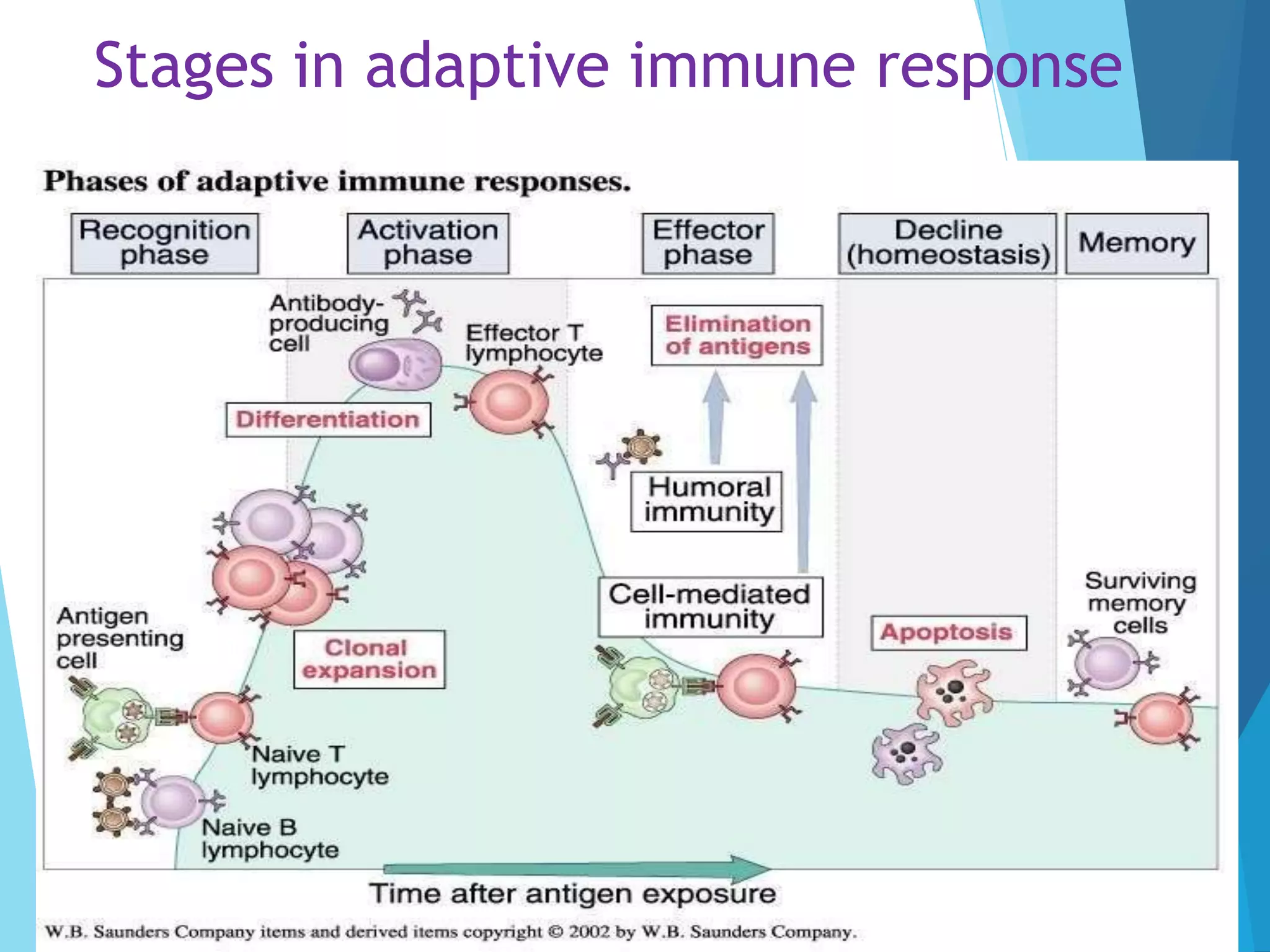
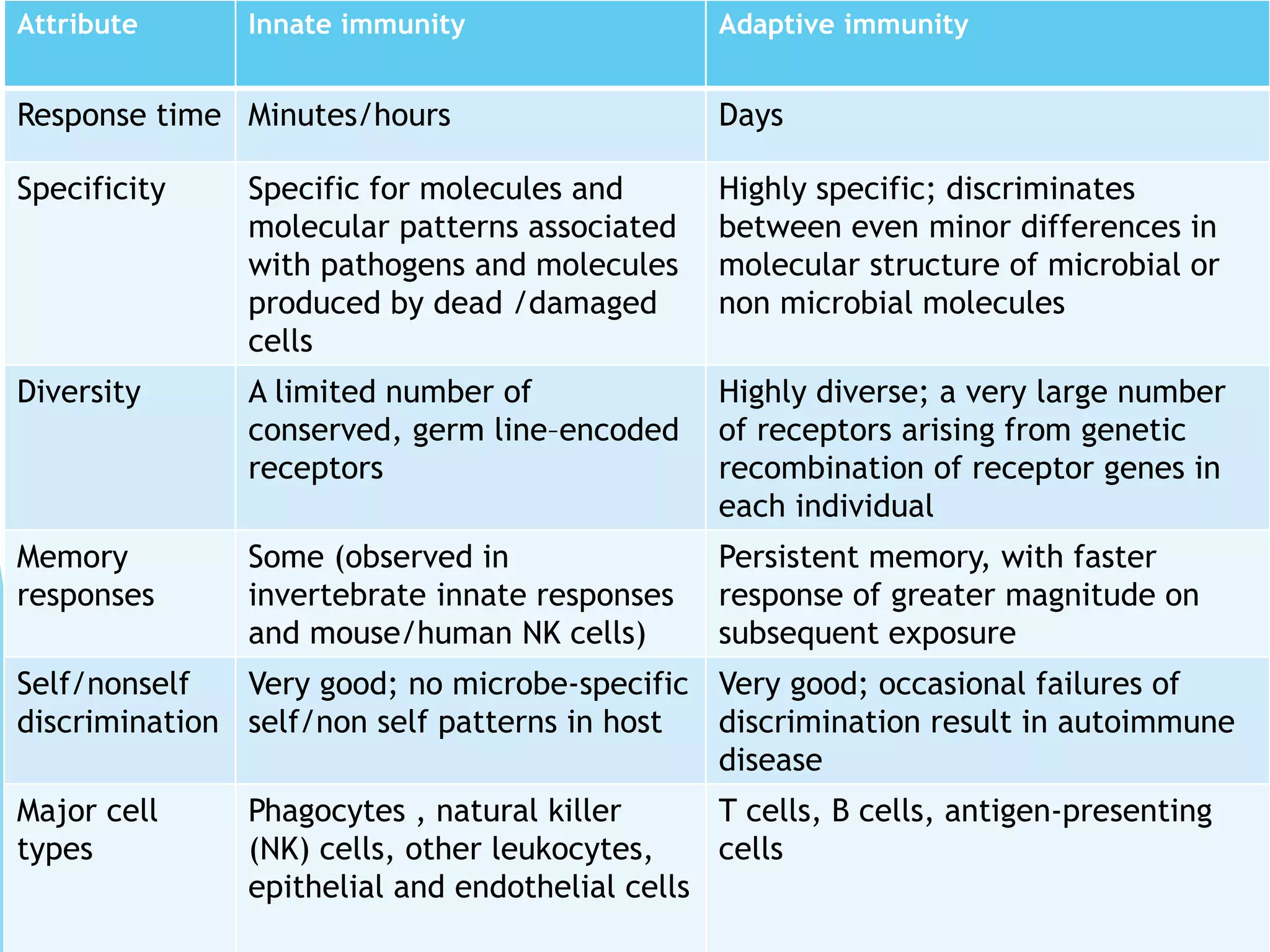
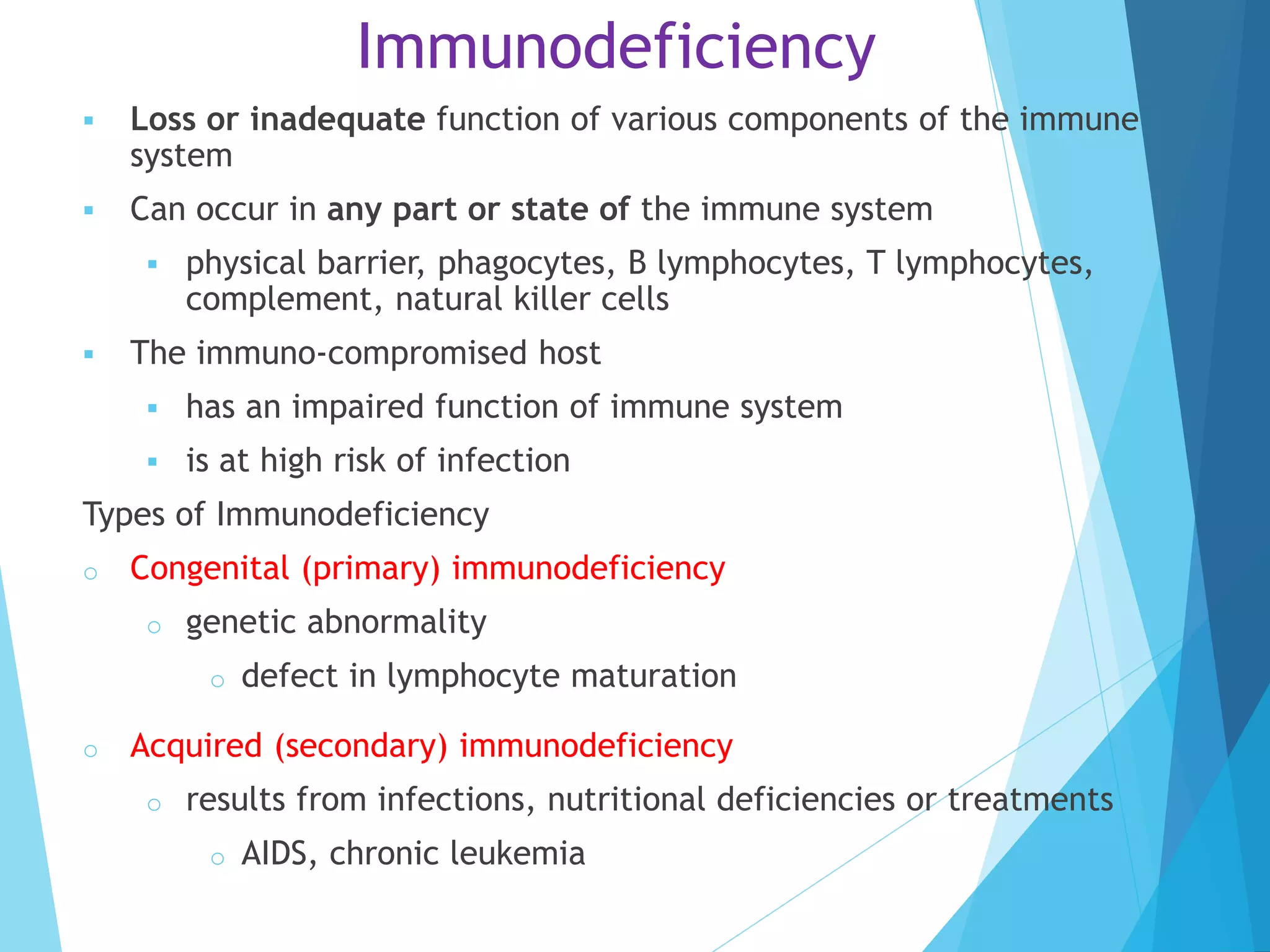
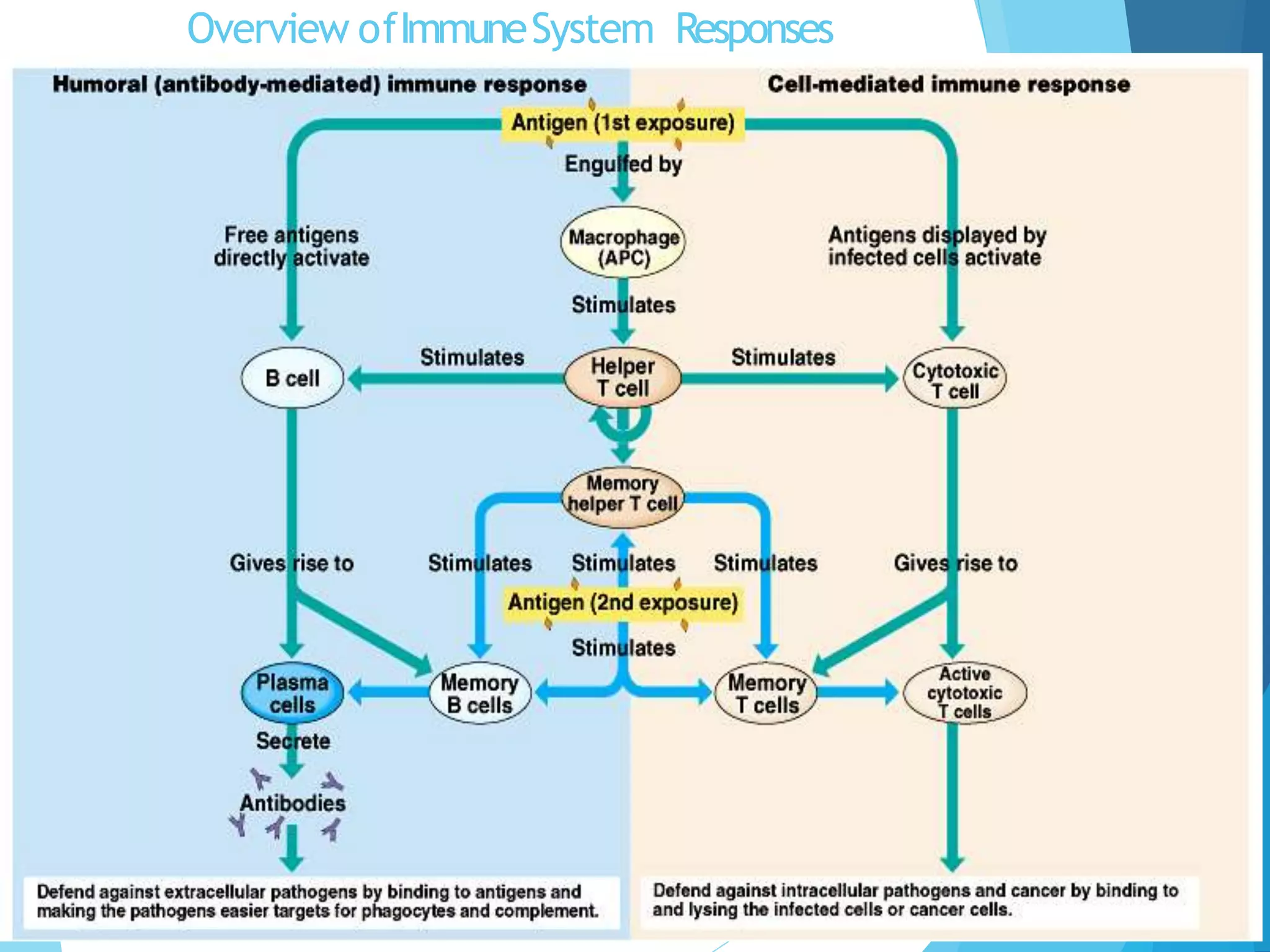
This document provides a detailed overview of adaptive immunity, describing its development, key functions, and mechanisms, which include both cell-mediated and humoral responses. It explains the roles of various immune cells, particularly T and B cells, as well as the processes of immune activation, memory response, and the importance of specificity and diversity in adaptive immunity. Additionally, it discusses herd immunity, types of immunodeficiencies, and the implications of immune responses and their failures.