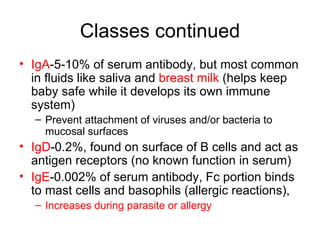
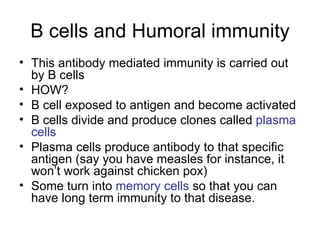
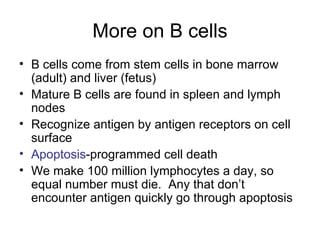
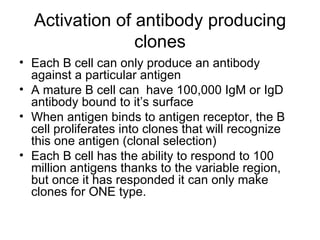
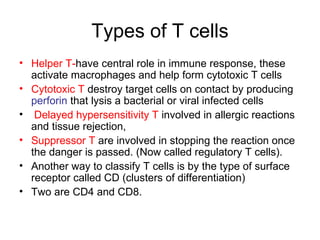
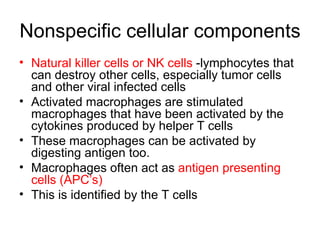
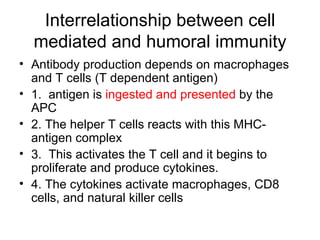
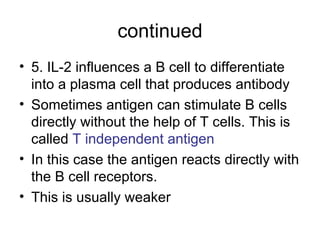
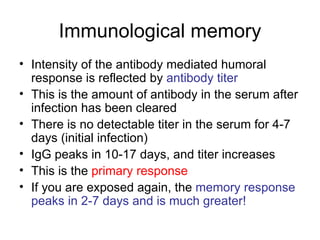
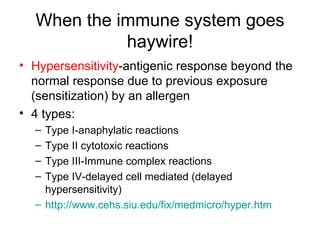
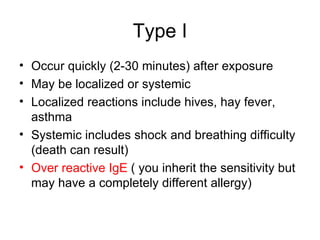
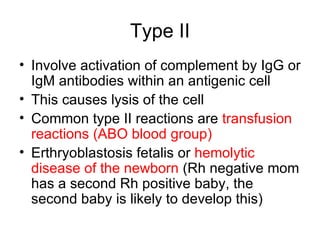
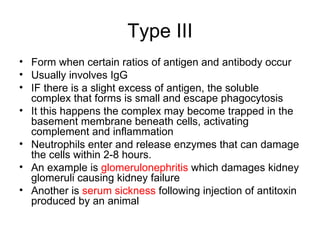
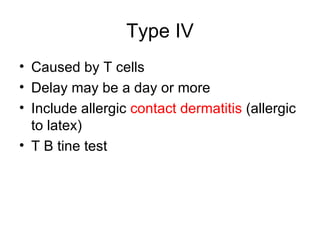
The document summarizes adaptive immunity and the immune system. It describes the two types of adaptive immunity - active and passive, which can be acquired naturally or artificially. It also details the roles of B cells and T cells in humoral and cell-mediated immunity, including antibody production, antigen recognition, and immune memory. Hypersensitivities are immune reactions beyond normal responses, classified into four types based on mechanisms.