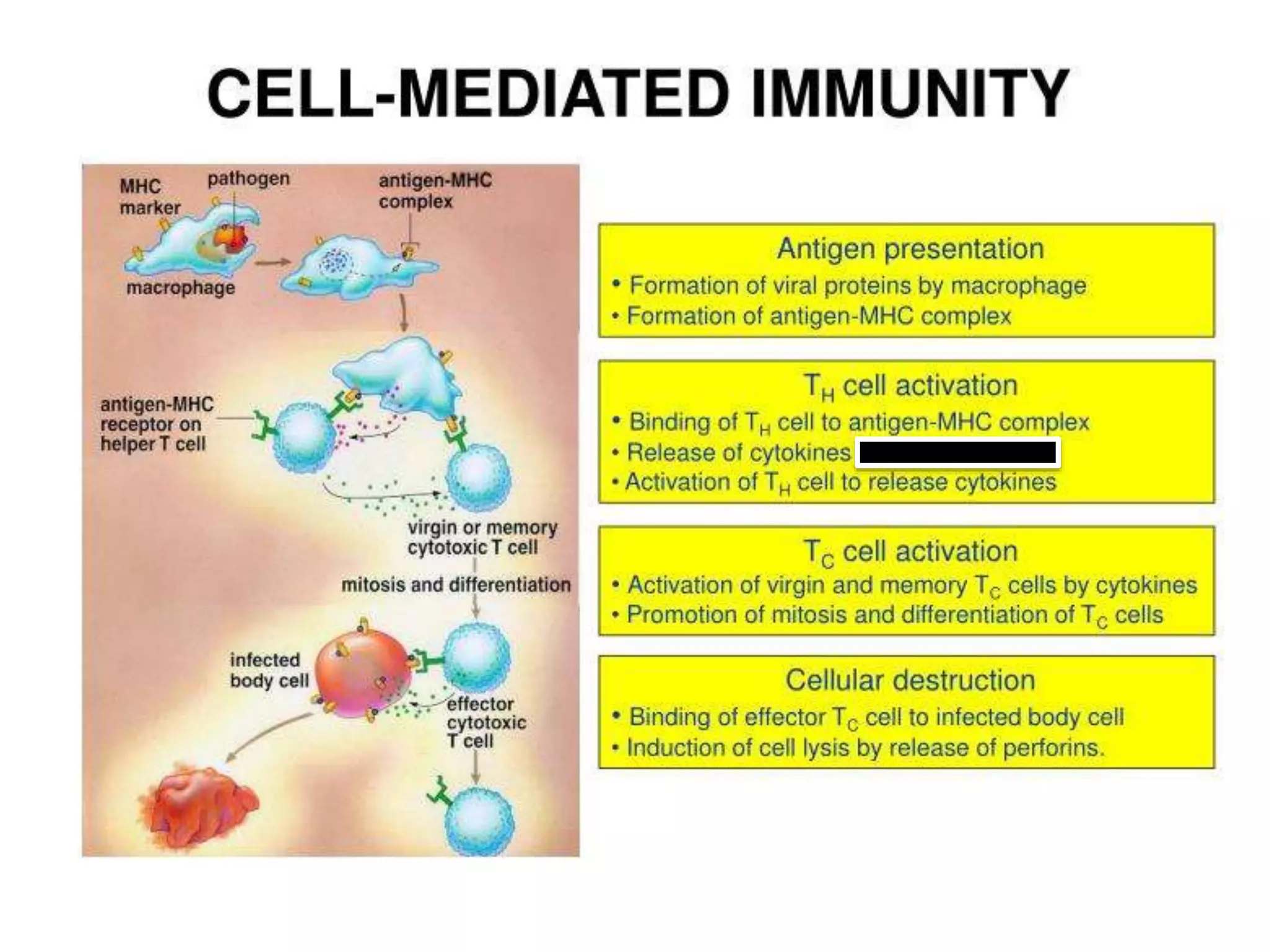
The document discusses adaptive immunity and the immune response. It describes the four phases of the adaptive immune response as encounter, activation, attack, and memory. Acquired immunity develops over one's lifetime from vaccines, infections, or antibodies from others. The adaptive immune response involves B cells, helper T cells and cytotoxic T cells. It also discusses the specificity, adaptiveness, discrimination between self and non-self, and memory properties of the adaptive immune response. The major cell types involved are T helper cells, cytotoxic T cells, T memory cells, and regulatory T cells. The roles and mechanisms of these cell types are described in detail.














![ T helper cell lineage development and function. The cytokines
produced by dendritic cells regulate the T helper cell lineage (Th1,
Th2, Th17, T regulatory [Treg], and follicular helper T cells
[Tfh]).
Each of them exhibits a unique phenotype, cytokine, and
transcriptional profile and exerts different functions in immune
response.
BCL-6, B cell lymphoma 6 protein;
CCR, C-C chemokine receptor;
CXCR, CXC chemokine receptor;
Foxp3, forkhead box P3;
RORs, retinoid-acid receptor related orphan receptors;
STAT, signal transducer and activator of transcription;
TGF-b, transforming growth factor-beta;
TNF, tumor necrosis factor](https://image.slidesharecdn.com/adaptiveimmunitytcells-221216090253-6cb6dcca/75/ADAPTIVE-IMMUNITY-T-CELLS-pptx-15-2048.jpg)