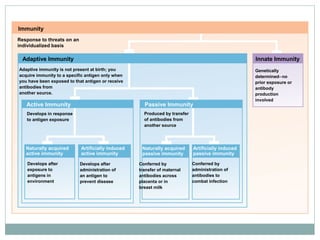
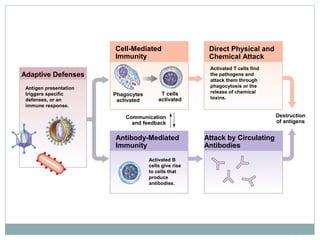
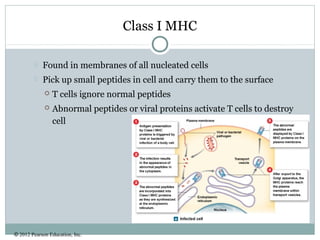
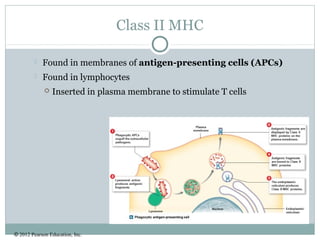
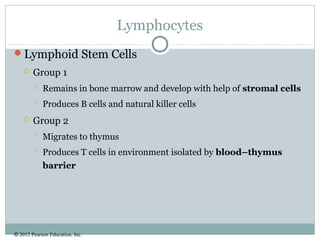
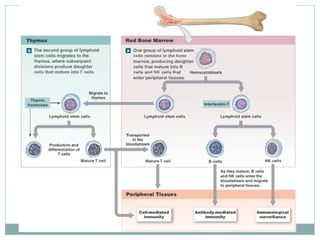
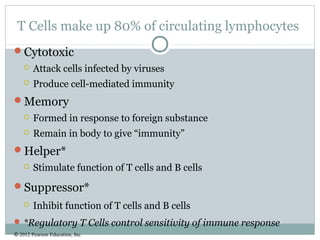
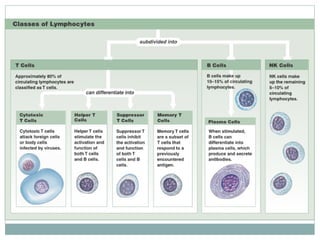
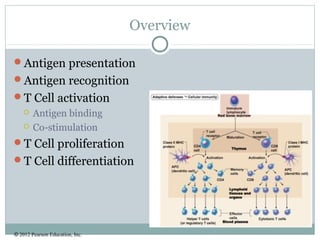
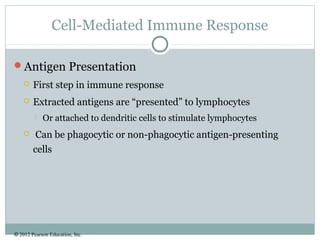
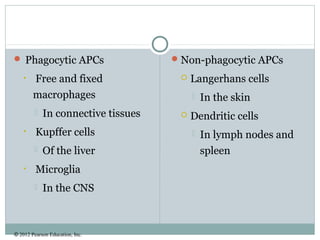
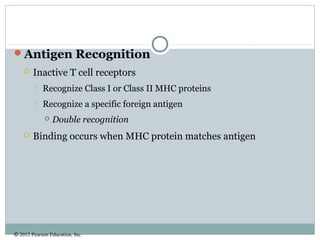
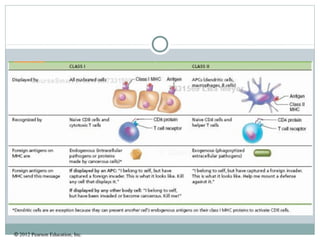
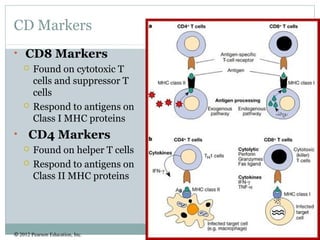
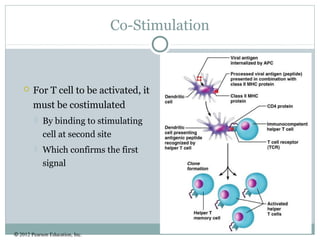
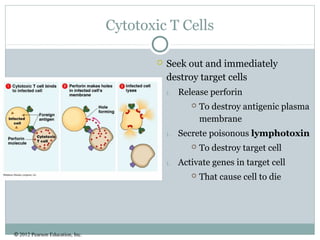
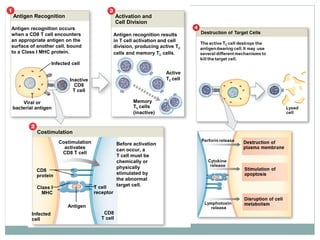
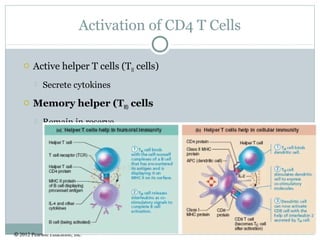
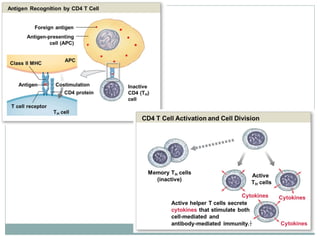
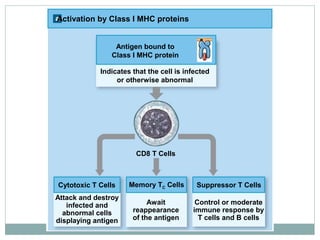
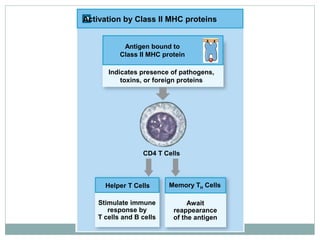
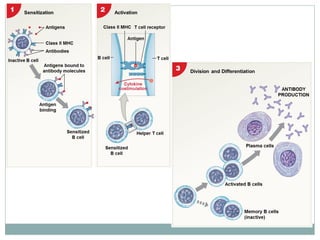
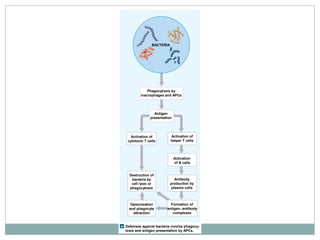
This document summarizes the key components of cellular immunity, including adaptive and innate immunity. It describes the properties of immunity, such as specificity and memory. The major topics covered are cytokines, MHC proteins, lymphocytes, antigen presentation, T cell activation, and B cell activation. Adaptive immunity involves cell-mediated responses by T cells and antibody-mediated responses by B cells. Innate immunity provides genetically determined defenses.