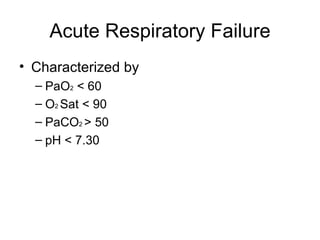
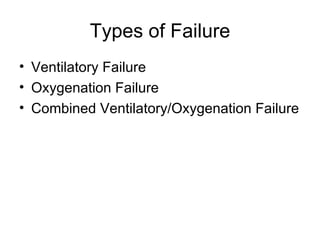
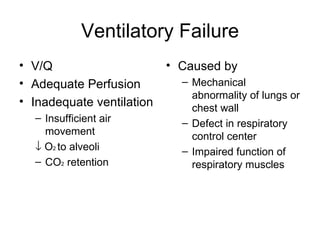
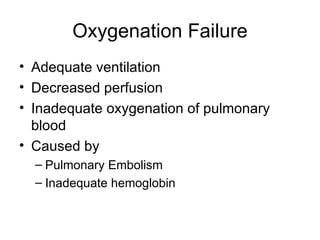
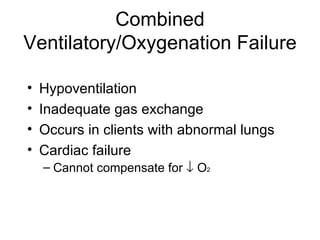
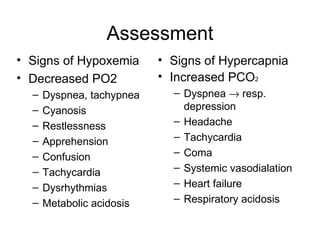
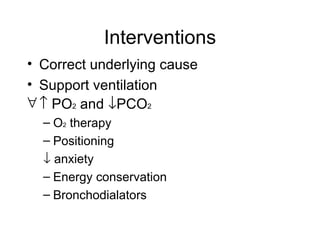
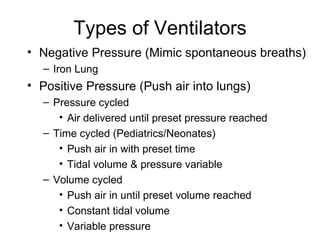
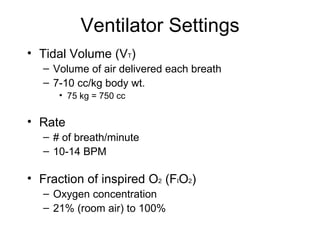
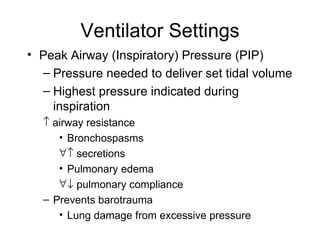
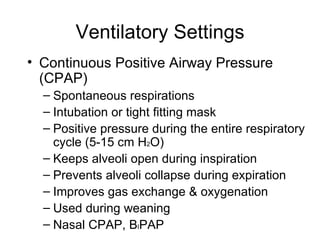
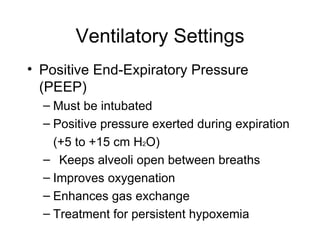
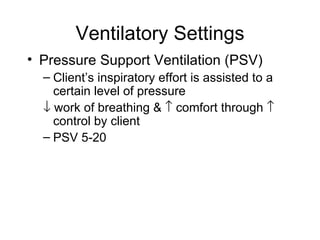
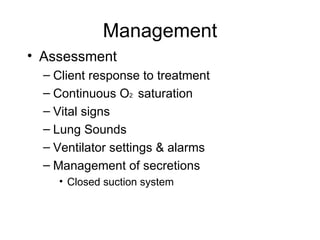
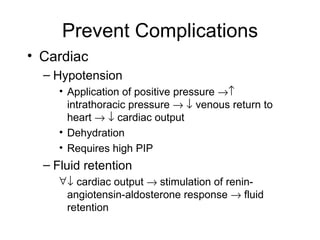
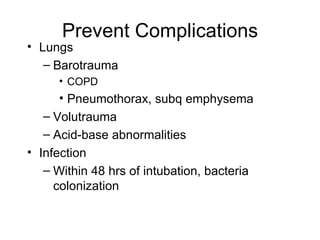
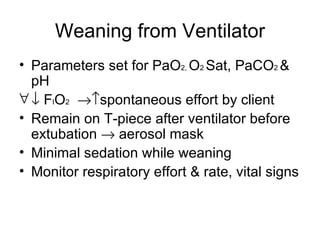
Acute respiratory failure is characterized by low oxygen levels and high carbon dioxide levels in the blood and can be caused by problems with ventilation, oxygenation, or both. Mechanical ventilation may be needed to support breathing and correct gas exchange abnormalities. Key settings on the ventilator include tidal volume, respiratory rate, oxygen concentration, and positive pressures. Close monitoring is needed to prevent complications and manage the underlying condition while optimizing the patient's ventilation and oxygenation.