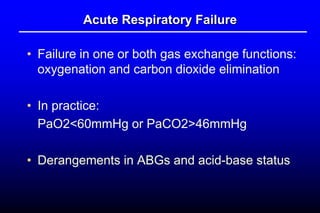
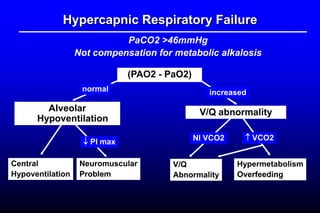
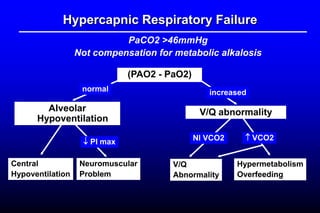
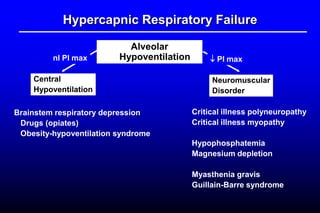
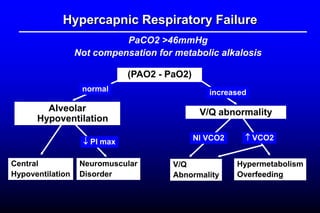
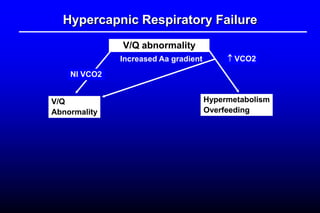
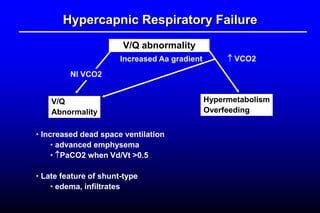
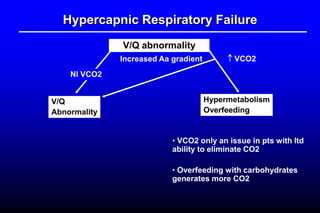
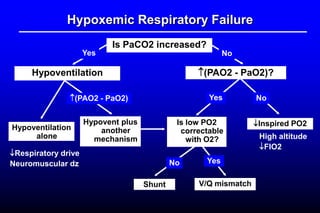
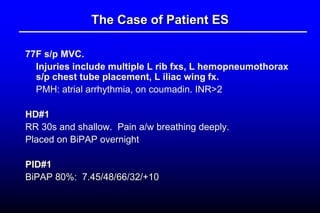
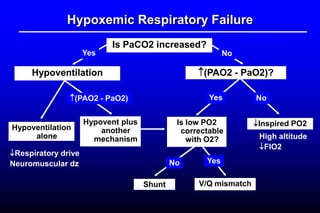
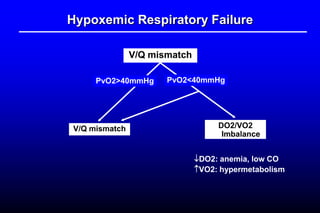
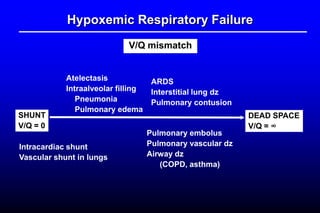
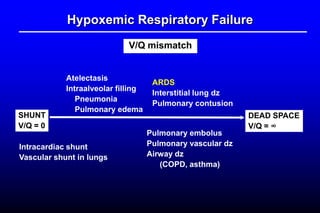
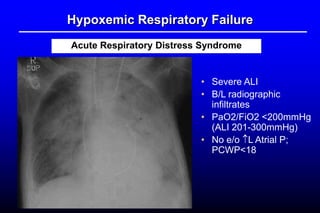
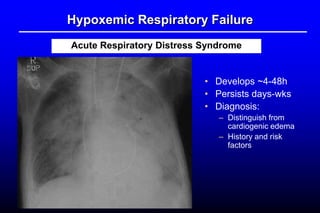
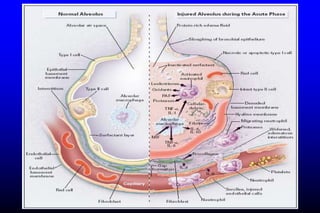
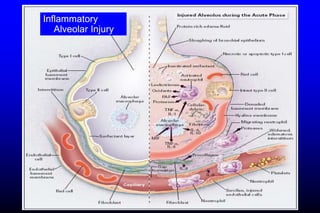
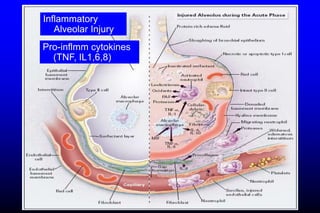
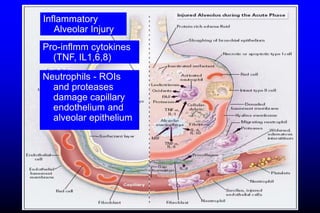
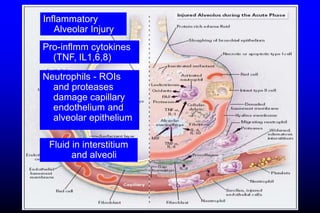
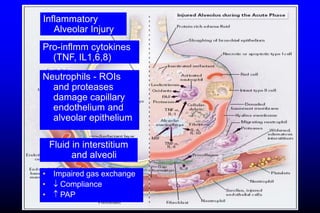
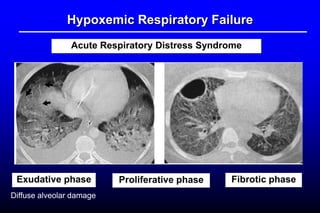
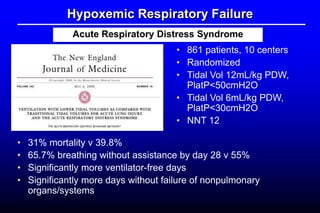
This document discusses a case of acute respiratory failure in a 300 kg patient who presented with sudden severe hypoxia and unconsciousness. It then provides an overview of acute respiratory failure, distinguishing between hypercapnic and hypoxemic respiratory failure. Various causes of each type are described in detail. The case is specifically focused on acute respiratory distress syndrome (ARDS), explaining its pathogenesis, risk factors, complications, and management including a landmark ARMA clinical trial showing benefit of lower tidal volumes.