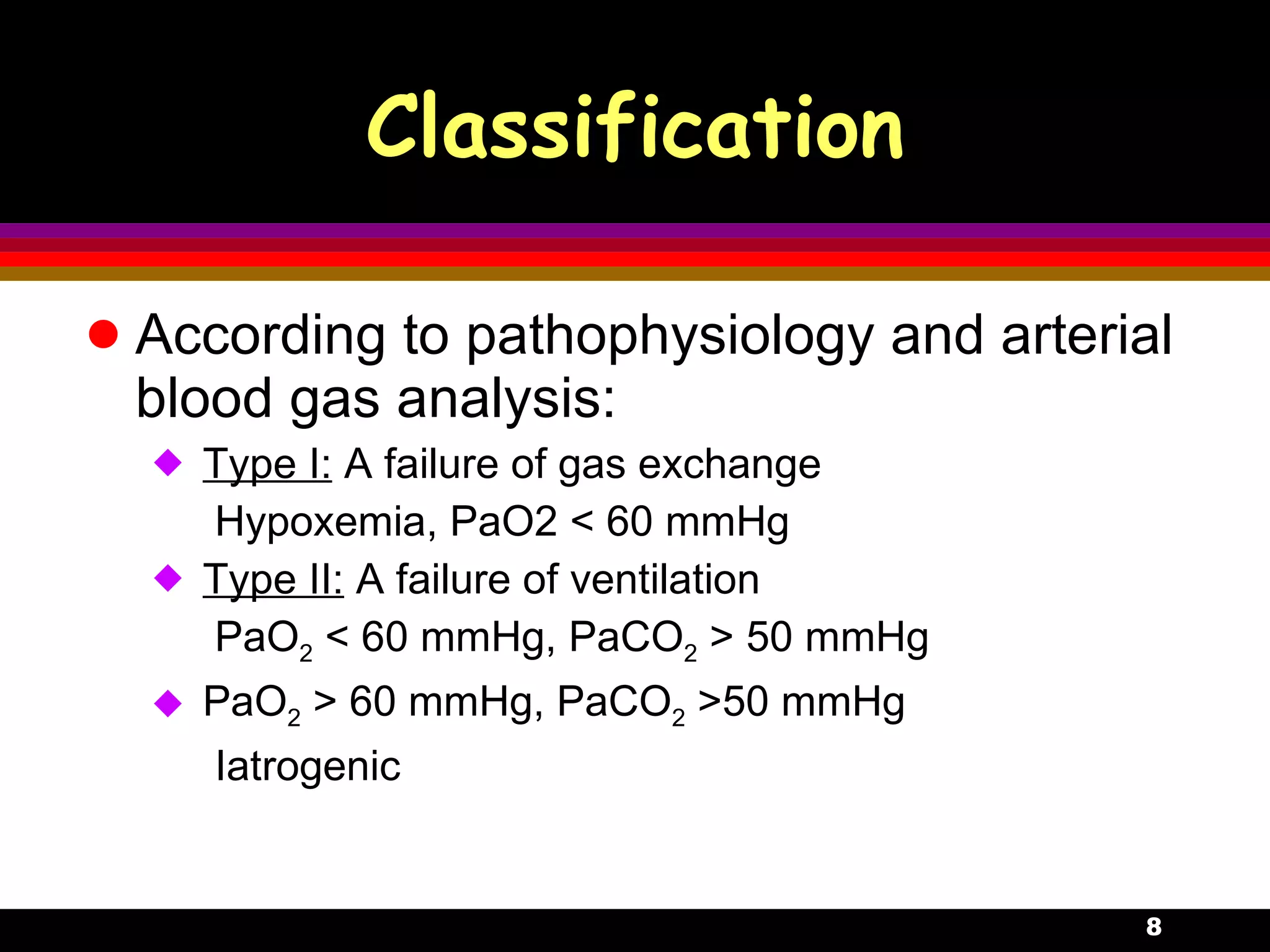
A 32-year-old male presented with fever, cough and sputum for 3 days. Chest X-ray showed pneumonia in the left lower lobe. Over the next few days, the patient developed acute shortness of breath and cyanosis. Blood gas analysis showed hypoxemia and acidosis, indicating acute respiratory distress syndrome (ARDS). The patient was intubated and received mechanical ventilation.























![Influence of hypercapnia Central nervous system Cerebral blood flow : PaCO2 0.133kPa , blood flow 4% -> headache, intracranial pressure Cerebrospinal fluid : H+ 、 HCO 3 、 CO 2 enter blood-brain barrier -> [H+] ->stimulate subcortex & excitability Consciousness : dizziness, asterixis, somnolence, coma, convulsion Peripheral nerves : sympathetic nerve, adrenal gland, distal nerves , catecholamine(CA) ](https://image.slidesharecdn.com/12-respiratoryfailure-100126025403-phpapp01/75/12-Respiratory-Failure-26-2048.jpg)








































