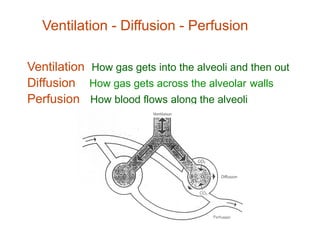
This document discusses indications for and goals of assisted ventilation as well as ventilator settings and modes. The key points are:
1. Assisted ventilation is indicated for respiratory failure, cardiovascular failure, neuromuscular failure, and airway protection. The goals are to provide optimal gas exchange while reducing work of breathing and risk of injury.
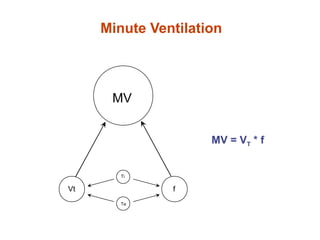
2. Initial ventilator settings depend on the underlying condition but generally involve a balance of pressures, rates, and oxygen levels to target appropriate oxygenation and carbon dioxide removal.
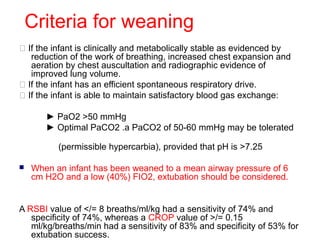
3. Common modes include assist-control, synchronized intermittent mandatory ventilation, and pressure support. Weaning involves gradually reducing support while monitoring blood gases and clinical stability.