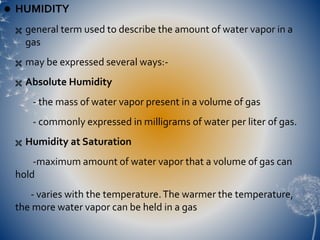
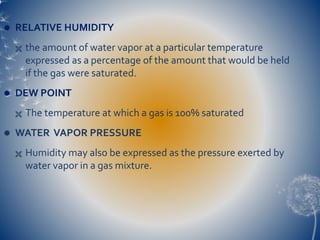
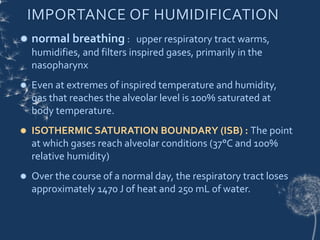
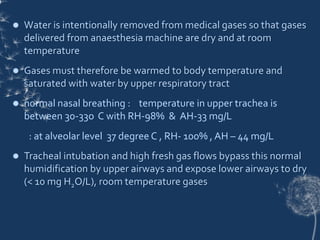
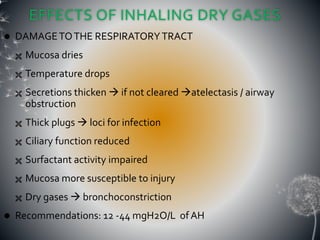
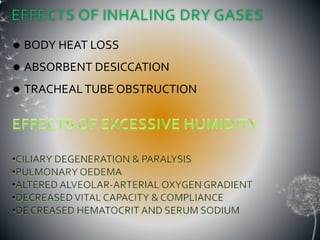
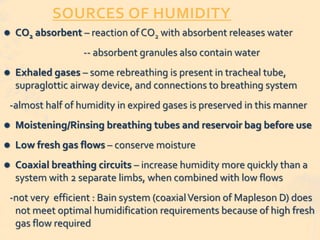
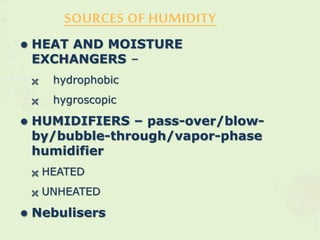
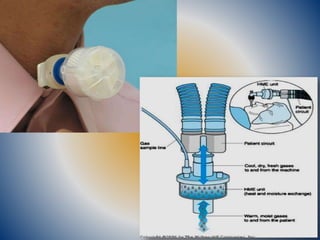
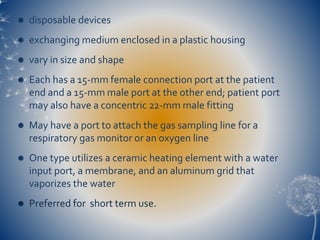
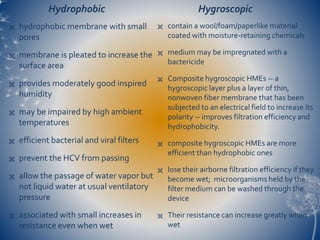
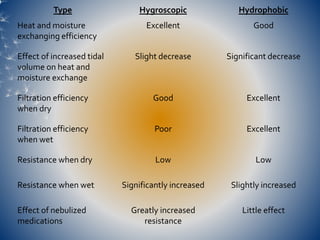
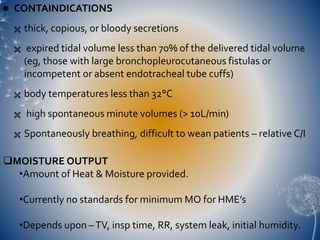
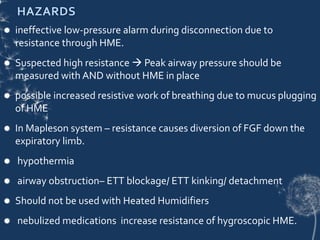
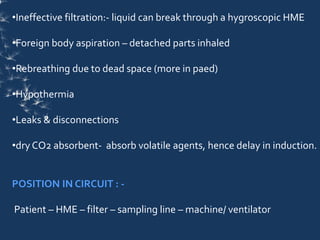
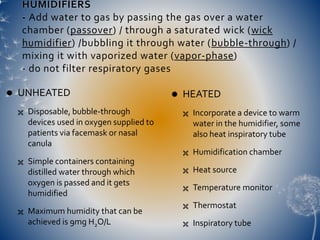
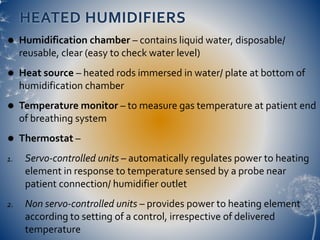
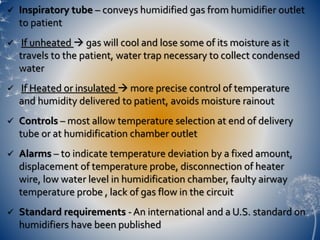
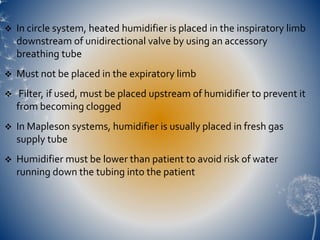
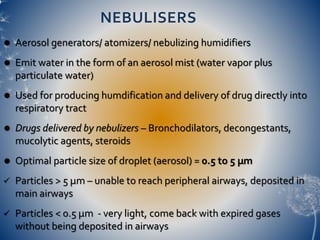
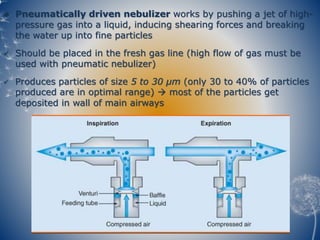
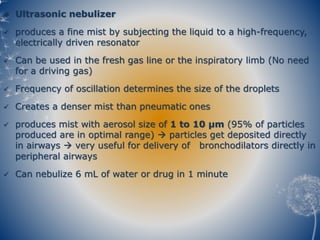
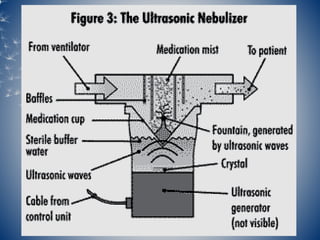
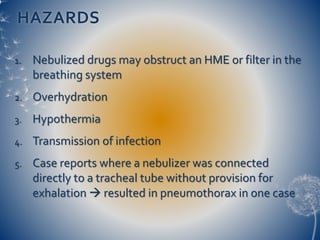
This document discusses humidification in the respiratory tract. It defines various humidity terms and describes how the upper airways normally warm and humidify inspired gases. When intubated, dry medical gases can damage the respiratory tract. Methods to add humidity include heat and moisture exchangers (HMEs), heated humidifiers, and nebulizers. HMEs are efficient but provide moderate humidity. Heated humidifiers can deliver saturated gases but require more maintenance. Nebulizers deliver medication directly but require high gas flows. Proper humidification is important to prevent respiratory complications.