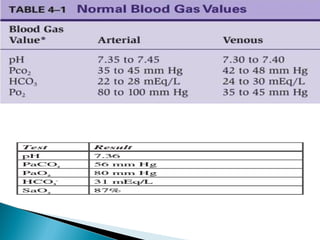
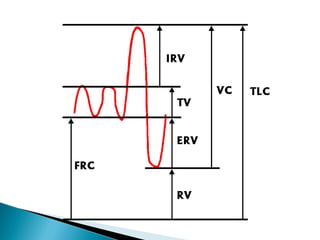
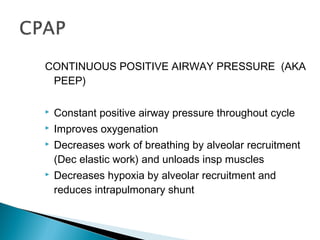
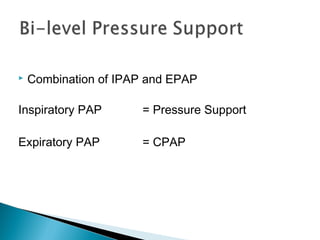
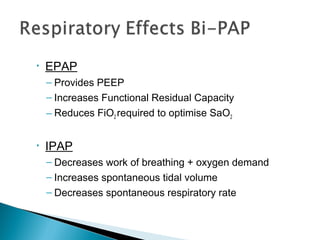
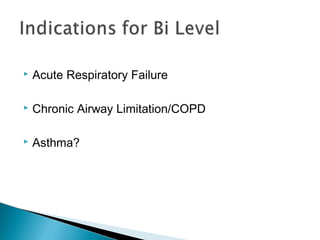
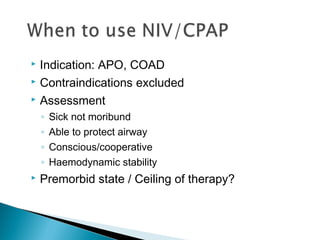
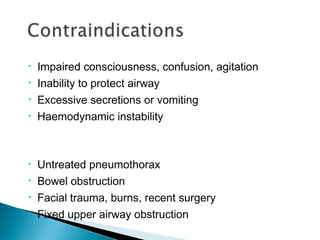
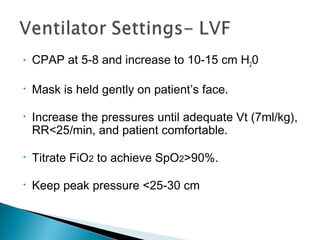
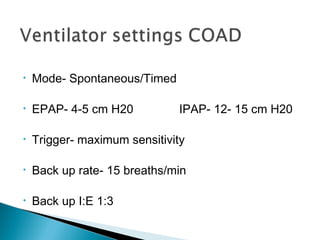
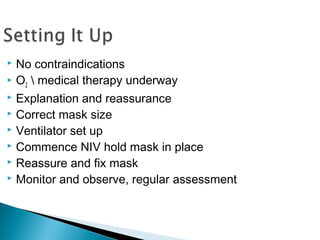
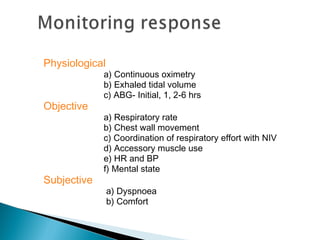
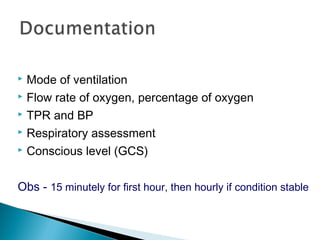
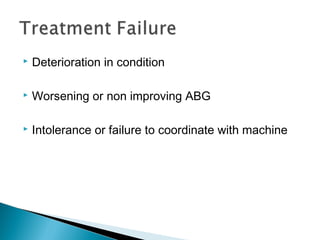
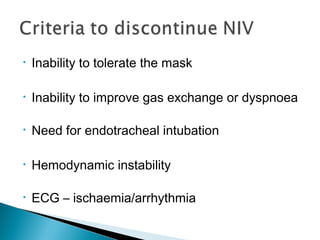
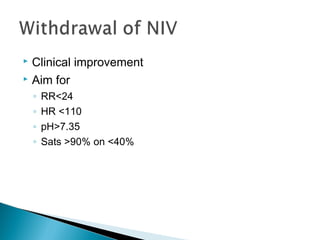
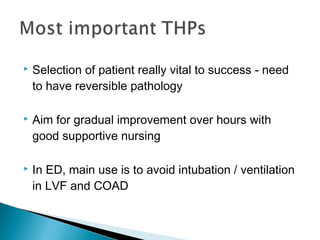
This document discusses non-invasive ventilation (NIV) including definitions, advantages, indications, contraindications and modes. It describes how NIV can improve gas exchange in respiratory failure by reducing work of breathing. Two main modes are described: CPAP and bi-level ventilation. Key points are that NIV can avoid intubation in acute respiratory failure if the patient is able to protect their airway and is hemodynamically stable. Close monitoring is needed and intubation may be required if the patient does not improve or deteriorates on NIV.