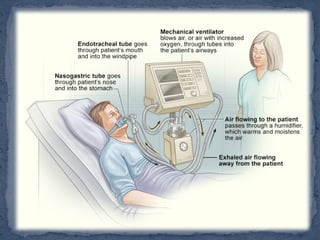
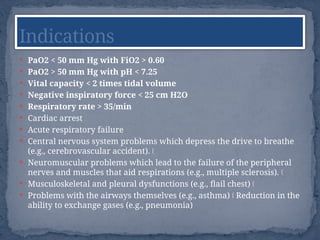
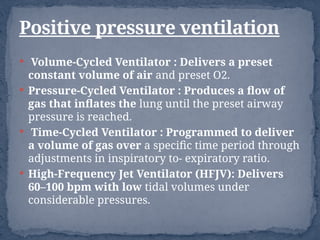
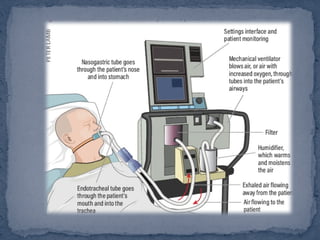
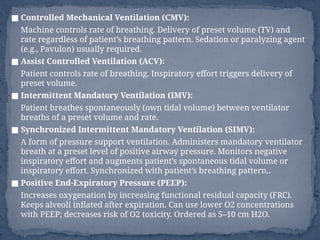
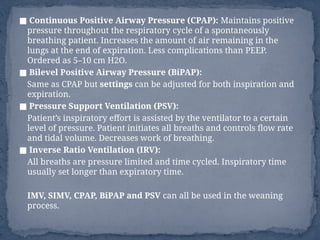
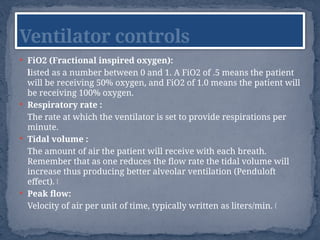
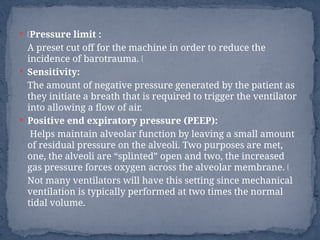
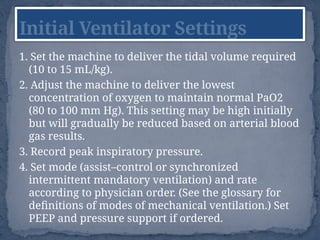
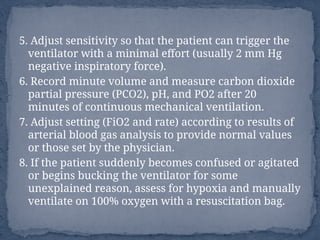
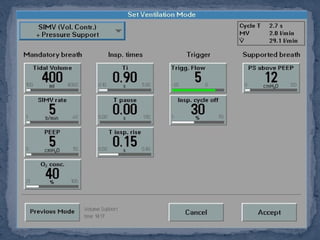
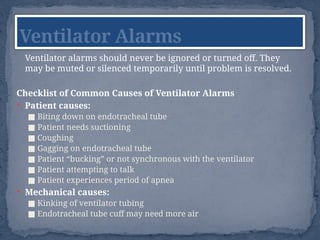
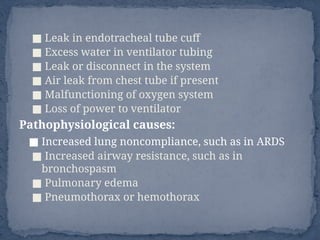
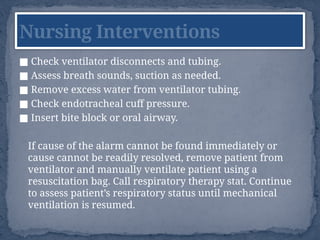
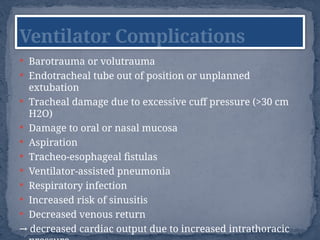
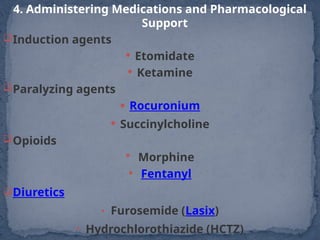
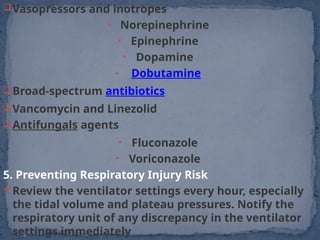
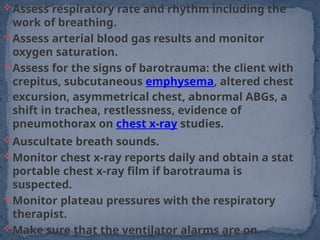
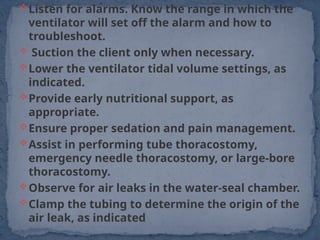
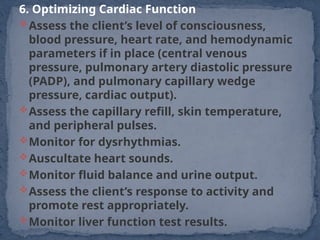
The document provides an extensive overview of mechanical ventilation in critical care, detailing the types of ventilators, modes of ventilation, indications for use, and settings required for patient management. It addresses the complications, nursing interventions, weaning criteria, and the pharmacological support necessary for patients reliant on mechanical ventilation. Additionally, it highlights the importance of continuous monitoring and assessment for effective management of ventilated patients.