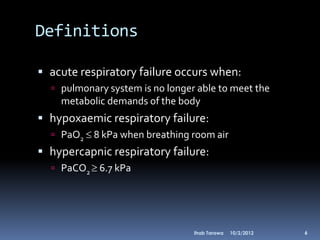
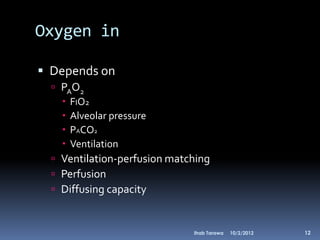
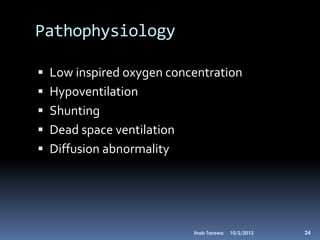
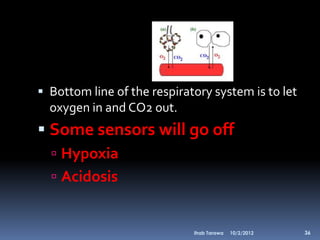
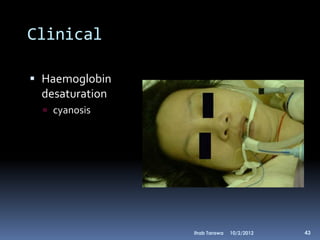
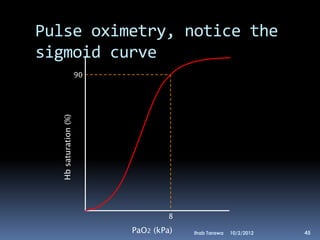
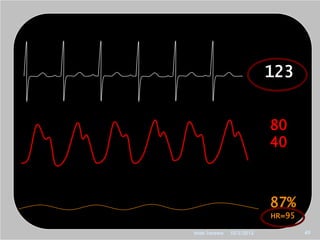
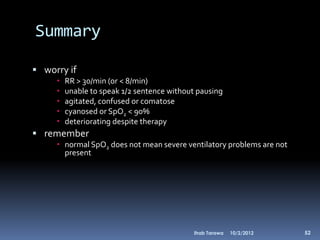
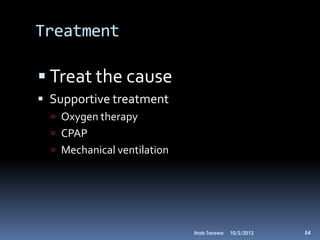
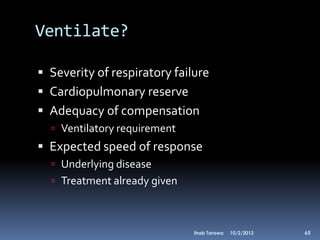
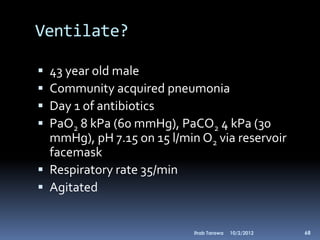
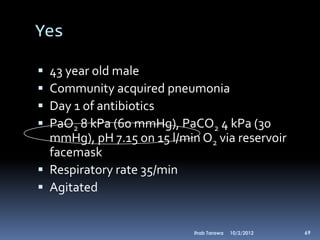
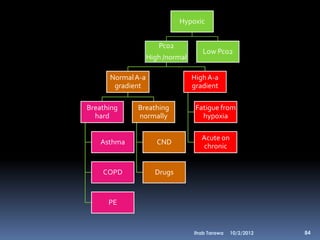
Based on the information provided, this patient is experiencing hypoxic respiratory failure and is not adequately compensating despite high-flow oxygen therapy. Mechanical ventilation would be indicated to support oxygenation and ventilation until the underlying pneumonia improves with treatment.