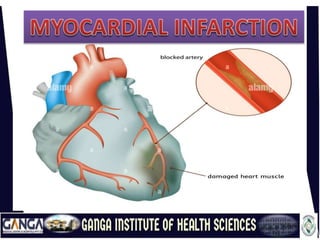
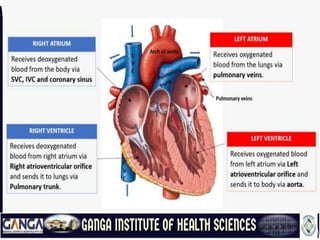
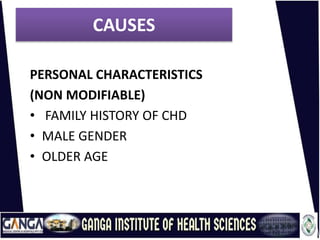
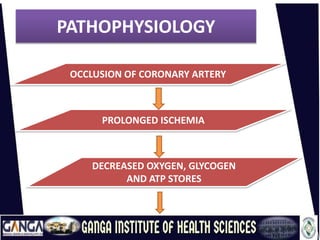
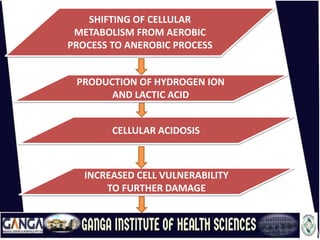
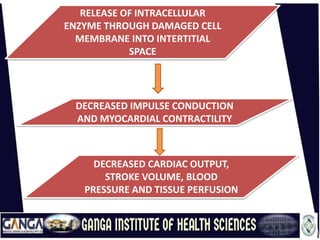
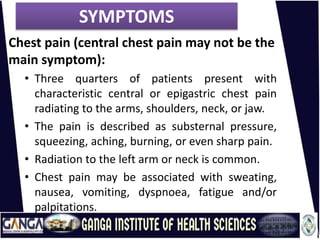
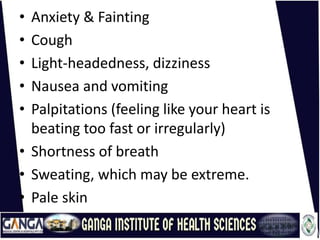
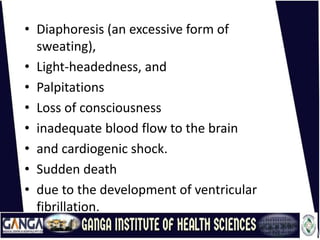
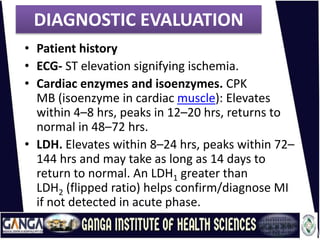
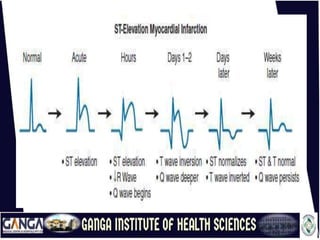
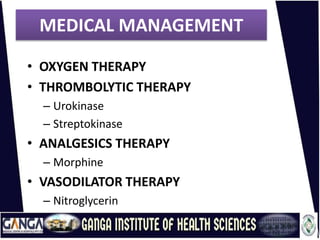
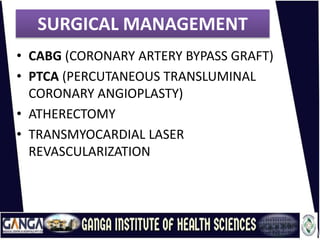
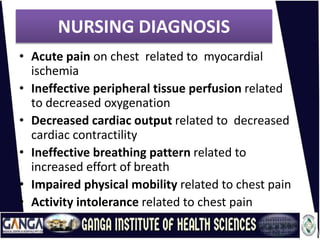
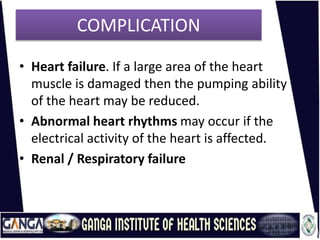
This document provides an overview of acute myocardial infarction (AMI or heart attack). It defines AMI as necrosis of heart muscle due to inadequate blood supply following coronary occlusion. The causes include lifestyle factors, physiological characteristics, disease conditions, and personal characteristics. The pathophysiology involves prolonged ischemia leading to cellular damage and dysfunction. Symptoms include chest pain and other signs of inadequate circulation. Diagnostic evaluation involves cardiac enzymes, electrocardiogram, imaging, and angiography. Management consists of oxygen, thrombolysis, analgesics, vasodilators, medications, and sometimes surgery. Nursing care addresses pain, perfusion, breathing, mobility, and activity tolerance. Complications can include heart failure and abnormal heart rhythms.